**This page contains affiliate links and our company will be compensated if you make a purchase after clicking on the links.
Black Men In America.com will be more aggressive in our efforts to educate the black community about the risks associated with a variety of cancers and other diseases that disproportionately affect our community. To this end we will use a wide range of resources throughout the health and medical industries, including high-quality sources, and peer-reviewed studies, to support the facts within our articles. We also fact-check and keep our content up-to-date.”
The resources on this page are not endorsed by Black Men In America.com, and we are not responsible for the content of or service provided by any of these resources.
Gary A. Johnson, Founder and Publisher
![]()
Small Shifts, Big Impact: Unconventional Paths to Better Mental Health

Mental health often gets framed in terms of grand interventions, but it’s the small, deliberate habits that can create profound change. You might already know the basics—sleep well, eat right, move your body—but the subtle, less-discussed practices can bring a different kind of balance. They work quietly, layering their benefits into daily life without demanding huge lifestyle overhauls. By leaning into creativity, sensory experiences, and connection with the world around you, you can create a network of support that feels organic. Here are seven approaches that step outside the usual self-care checklist, offering fresh ways to care for your mind.
Morning Light Ritual
The early hours carry a distinct quality of light that sets the body’s internal clock and lifts mood. A few minutes of basking in early sunlight can signal your system to release hormones that regulate energy and improve focus. It’s not about exercise or productivity—though those may follow—but simply letting that sensory cue anchor your day. This light exposure has a grounding effect, making the rest of the morning feel less rushed and more intentional. Over time, mornings shift from being a hurdle to becoming a moment of quiet renewal.
Curated Sensory Design
What surrounds you has a direct line to your emotional state. The sounds, scents, and textures in your environment shape how you experience each moment, often without you realizing it. By introducing intentional elements—soft fabrics, warm lighting, scents that signal calm—you create a subtle backdrop for mental ease. This is not about a single purchase or a decor trend, but an ongoing practice of tuning your space to the moods you want to cultivate. Over time, these micro-adjustments can make your home or workspace feel less like a backdrop and more like an ally in maintaining balance.
Natural Stress Relief
Reducing stress can be as much about choice as it is about method. Magnesium supports muscle relaxation and encourages a calmer nervous system, making it easier for the body to let go of tension. Lavender oil works through scent, activating pathways in the brain that help lower anxiety and promote a sense of ease. THCa offers a plant-based option, and this is worth a look if you’d like the soothing effects without the intensity associated with other cannabinoids. Together, these three options create a versatile toolkit that can be adapted to suit different needs and preferences.
Junk Journaling
Creativity can be a powerful form of release, especially when perfection isn’t the goal. Junk journaling turns everyday paper, ticket stubs, and textures into something personal and expressive. It’s part creative outlet, part quiet reflection, with the process itself being as valuable as any finished piece. This tactile, playful approach can help shift perspective, replacing mental heaviness with lightness. Over time, the practice becomes a personal archive of mood, memory, and quiet self-discovery.
Nature Therapy
Spending time in green spaces works on the mind in ways science is still uncovering. Letting nature set the pace—whether in a forest, park, or garden—can dissolve mental clutter and make room for grounded thoughts. It’s not about hiking for miles or chasing views, but about slowing down enough to notice details like the texture of bark or the movement of shadows. This unhurried presence is difficult to replicate indoors, and even brief contact can shift your baseline stress levels. Over time, these moments accumulate into a subtle but powerful form of restoration.
Laughter Yoga
Laughter yoga blends intentional laughter with yogic breathing to create a quick shift in mood and energy. Sessions usually start with playful warm-ups, clapping, and breathing exercises before moving into sustained bouts of laughter. Even if it feels forced at first, the physical act of laughing can trigger the body’s natural release of endorphins, lowering stress levels. In group settings, the rhythm builds as participants laugh their way to relief, often turning simulated laughter into the genuine kind. The mix of movement, breath, and shared joy leaves most people feeling lighter, more connected, and refreshed.
Surf Therapy
The ocean offers both exhilaration and calm, drawing you into the present moment. For many, catching waves is both literal and symbolic, blending the thrill of movement with the sensory immersion of saltwater and sky. Surf therapy demands focus, coordination, and patience, leaving little room for mental noise. Even for beginners, paddling out can reset perspective, shifting attention away from day-to-day stress. Over time, the ocean becomes not just a place of recreation but a trusted space for renewal.
Mental health thrives on habits that are consistent yet flexible, personal yet connected to something larger. Whether it’s sunlight on your skin, paper under your fingertips, the hush of a forest, or the sound of shared laughter, these practices root you in moments of genuine presence. You don’t need to overhaul your life to feel a difference—you need only to make space for experiences that engage both body and mind in meaningful ways. The beauty of these approaches is that they require no single skill set, no rigid schedule, and no perfect execution. They ask simply for your attention, and in return, they offer balance, perspective, and a renewed sense of connection.
Discover insightful stories and empowering discussions at Black Men In America, where voices resonate and perspectives inspire change.
Photo credit: Image: Pexels
![]()
5 Reasons Why Home Massage Tools Are a Game-Changer for Wellness

There’s no denying it—massage therapy feels amazing. But it’s more than just a feel-good luxury. According to the Mayo Clinic, massage therapy can help with everything from reducing stress and improving circulation to easing chronic pain. They’re even linked to better sleep and enhanced immunity.
The catch? Regular massages from professionals aren’t cheap. And unless you live next to a spa or clinic, they can be hard to schedule consistently. That’s where home massage tools come in. These simple, often affordable devices give you the benefits of massage without the hassle, right in your living room.
In this guide, we’ll explore five key reasons why home massage tools can level up your wellness routine, followed by a rundown of five tools worth considering for your personal toolkit.
5 Reasons Why Home Massage Tools Are a Game-Changer for Wellness
1. Everyday Stress Relief, Anytime
Stress doesn’t wait for your next spa appointment. Whether it’s tension from work, parenting duties, or just general life pressure, stress settles into your body. Home massage tools can step in when you need immediate relief. A quick 10-minute session with a neck or foot massager can help lower cortisol levels and encourage your body to relax. No need to book in advance. No tip required.
2. Support for Muscle Recovery and Soreness
If you work out regularly—or even just live an active lifestyle—chances, are you deal with sore muscles. Massage tools like percussive guns and rollers promote blood flow to tired or tight areas. This not only helps reduce inflammation but can speed up recovery. So, instead of skipping workouts because you’re sore, you can bounce back faster.
3. Posture Support and Pain Prevention
Poor posture can silently wreak havoc on your body. The risks of bad posture go beyond just back and neck pain—it can mess with your breathing, digestion, and mood. Home massage tools can target tight muscles around your spine, shoulders, and hips that contribute to misalignment. Regular use can help your body stay upright and pain-free throughout the day, especially if you spend hours at a desk.
4. Saves You Time and Money
Massage therapy is often priced out of reach. With tools at home, you’re making a one-time investment that you can use repeatedly. No commute. No waiting rooms. No co-pays. It’s a smart, budget-conscious way to stay committed to your wellness routine over the long term.
5. Customizable Comfort
Everyone’s body is different. One of the underrated perks of home massage tools is that you control the intensity, duration, and area you want to focus on. Whether you prefer a gentle vibration or deep tissue kneading, there’s a tool that matches your needs, without explaining your preferences to anyone else.
5 Massage Tools to Consider for Your Home Setup
1. Percussive Massage Guns
These have taken the wellness world by storm—and for good reason. A percussive massager offers rapid pulses that dig into deep tissue, making it ideal for athletes or anyone with tight muscle groups. They come with adjustable speeds and interchangeable heads so you can target different parts of the body with precision. Among the selection on QVC, you can even find models from brands like Sharper Image, which have various attachments to tailor your experience.
Note: If you deal with chronic muscle tension, this might become your favorite recovery tool.
2. Shiatsu Neck and Shoulder Massagers
These tools mimic the kneading action of a real massage therapist, making them a popular choice for people with neck stiffness or upper back tension. They’re often designed to wrap around your shoulders and can be used while sitting on the couch or working at your desk. The brand TRAKK even uses memory foam cushioning, so you can snooze while using this massager.
Look for: Heat settings and adjustable pressure options for a more personalized experience.
3. Foot Massagers
Don’t underestimate the power of a good foot massage. A quality foot massager can relieve tension not only in your feet but throughout your whole body. This is especially helpful if you’re on your feet all day or suffer from plantar fasciitis. If you’re willing to go the extra mile, the manufacturer Homedics’ collection of foot massagers includes ones that even deliver acupressure with ventilation for enhanced indulgence.
Pro tip: Go for models with rolling nodes and heat for maximum effect.
4. Foam Rollers
Foam rollers are a classic for a reason. According to Harvard Health, foam rollers help relieve muscle tightness and improve flexibility. Perfect for post-workout recovery or decompressing after a long day, foam rollers work by using your own body weight to apply pressure. They’re especially great for your thighs, calves, and back. If you’re unsure how to use a roller properly, makers such as GoFit come with a training manual to make the experience easier and safer.
Tip: Choose a roller with medium firmness if you’re new to it—it’s a great starting point before trying textured or harder options.
5. Massage Cushions or Chairs
For a full-body experience, massage cushions or chair pads can be placed on your sofa or office chair. They often offer vibration, rolling, and heat features that target the back, shoulders, and sometimes even the glutes. Although they do cost a pretty penny, they’re often investment pieces since they’re made to last. For instance, Osaki massage chairs also come with a three-year warranty, so you really get your money’s worth.
Bonus: Some massage chairs offer presets based on common issues like lower back pain or general fatigue.
Final Thoughts
You don’t have to be a pro athlete—or drop serious cash—to enjoy the benefits of regular massage. Investing in home massage tools is one of the smartest moves you can make for your wellness. They’re convenient, effective, and a great way to support your health journey without leaving the house.
With so many options on the market, you can find the right tool to fit your lifestyle, body needs, and budget. Whether you’re managing stress, improving your posture, or speeding up muscle recovery, a little daily massage can go a long way.
Article written by Rose Henderson exclusively for Black Men In America.com.
![]()

2. Constipation. Poor posture on a toilet — hunched over with your knees lower than your hips — can promote constipation. “That position closes the anus somewhat and makes it harder for the abdominal muscles to help move feces out,” Markowski says. Constipation is characterized by fewer than three bowel movements per week; hard, dry stools; straining to move the bowels; and a sense of an incomplete evacuation.
3. Heartburn and slowed digestion. Slouched posture after a meal can trigger heartburn caused by acid reflux (when stomach acid squirts back up into the esophagus). “Slouching puts pressure on the abdomen, which can force stomach acid in the wrong direction,” explains Dr. Kyle Staller, a gastroenterologist at Harvard-affiliated Massachusetts General Hospital. “And some evidence suggests that transit in the intestines slows down when you slouch. In my opinion, it probably does play a small role.”
The Prevalence of Hearing Loss Among Black Men in America

There are a variety of factors that can lead to the development of hearing loss. However, one thing we should keep in mind when considering hearing loss is one’s race. A recent study on the social determinants of health and hearing loss in American adults emphasizes that, while hearing loss can be exacerbated by factors such as aging and genetics as well as other illnesses, there are also non-medical, societal factors that can influence the condition.
In the study, researchers found that non-Hispanic Black participants had half the odds of hearing loss as non-Hispanic White participants. However, the study also noted other societal factors, such as lower education level, as being crucial factors impacting hearing loss development. For example, those without a high school diploma had double the odds of hearing loss compared to college graduates or above. Likewise, income level also plays a role in the likelihood of developing hearing loss.
However, previous studies have highlighted the importance of race in hearing loss discourse. In 2022, researchers noted that, while hearing loss is less prevalent in Black individuals, the relationship between hearing loss and dementia is stronger in the Black community. The study also highlighted that hearing loss is a risk factor for dementia despite the lack of race-based studies on the subject. Below, we’ll take a closer look at hearing loss among Black men in America and the various hearing technologies and solutions that can help bridge the gap:
Hearing loss among Black men in America
According to data from the Hearing Health Foundation, nearly two million Black Americans have a hearing impairment. As mentioned in our introduction, hearing loss rates are noticeably lower in Black individuals than their White counterparts. Research has shown that Black Americans 65 years and older have much better hearing than older White adults. However, this doesn’t mean they are exempt from it. As of 2022, there are still almost two million Black Americans suffering from hearing loss. Notably, researchers also found that among men, non-Hispanic Black Americans have a prevalence of hearing loss that is similar to non-Hispanic White Americans who are ten years younger.
While more studies are certainly needed to determine why hearing loss is less prevalent in Black American men than their White counterparts, researchers propose that differences in lifestyle habits may also play a role. For example, factors such as diet, smoking habits, noise exposure, bone density, and cochlear melanin content have been noted as potential explanations for the disparity in hearing loss prevalence.
Hearing technologies and solutions
In recent years, there has been a rise in emerging and advanced technologies promising to make hearing loss treatment more effective and accessible for all. Aside from current hearing loss treatments such as hearing aids and cochlear implants, for example, researchers have worked on developing new technologies like gene therapy and stem cell therapy, as well as regenerative medicine that can regenerate hair cells and stimulate the growth of new auditory nerve cells.
In terms of advancements in hearing aid technologies and solutions, various tech and wearable companies are committed to revolutionizing hearing aid technology. Nuance Hearing has been innovating on traditional hearing devices through the company’s hearing glasses, the aptly named Nuance Audio. Marketed as an over-the-counter hearing aid integrated into smart glasses, the Nuance Audio mixes sound engineering and world-class smart eye wear design for a stylish, high-tech solution to hearing loss and impairment.
Aside from the Nuance Audio smart glasses, other tech giants are looking to contribute to the market. Apple recently announced that part of its flagship headphones, the AirPods Pro 2, will introduce all-new hearing health features via a free software update. This includes a hearing test as well as hearing protection and hearing aid capabilities. Using the new AirPods Pro 2 update, users will be able to take clinically validated hearing tests and benefit from hearing health features like loud sound reduction.
If you enjoyed this post and would like to learn more about enhancing health for Black men, you may enjoy our previous post on the importance of cultivating mindfulness in pursuit of contentment, gratitude, and movement. Likewise, you can also check out our homepage for more news and insights relevant to the community.
Article written by Rose Henderson, exclusively for BlackMenInAmerica.com
Image source: https://www.pexels.com/photo/man-in-white-tank-top-sitting-on-concrete-floor-3766228/
One Man’s Struggle and Success Losing Weight
Posted July 30, 2024
By Gary A. Johnson – Publisher (Black Men In America.com)
Posted: July 30, 2024
Warning: The response to my Facebook post about my weight loss struggle has been somewhat emotional and overwhelming. Some folks have emailed me offline to thank me for putting myself out there and giving them hope. One friend said that she had all but given up on trying to lose weight, but after reading my post, she is going to start walking again, and toss out the junk snacks in her pantry. I received 8 supportive emails over the past 24 hours. I know what it feels like to try and lose weight. In the spirit of helping others, I feel very little risk in sharing the following for the first time.
I’ve been overweight for 20 years. I started gaining weight in 2004. In August of 2011, I hit the 300 lb. mark. In 2016, I weighed 350 lbs. During those 20-years, part of my struggle included poor eating choices, overeating, and not exercising—all of which I own and take responsibility for not handling my business. The biggest barrier to becoming healthy was not understanding that I was an emotional eater. I knew that I was not eating healthy but used food as a coping mechanism. Listening to people who tell you that you are fat and joking about your weight was difficult. I never felt that the comments were purposely mean-spirited to hurt my feelings. I believed that the people making the comments believed they were trying to help me and motivate me to get slimmer.


Most of the negative comments came from my family and friends, including my mother (who reeled off a slew of solid one-liners over the years). Here are a few “fat shaming” comments that I vividly remember from friends and family:
- “Man, you getting’ so big we gonna have to put 3 numbers on the back of your jersey.”
- “When is the baby due?”
- “Looks like you’re in your 3rd”
- “I thought you said you were losing weight. It doesn’t look like it to me.”
- “I don’t understand why you are so big. Just stop eating.”
Fortunately for me, the effects of these comments did not have an impact on my self-esteem, but it did add to my existing stress of being a working husband and father with a stressful job and a long commute in rush hour traffic.
As I continued to gain weight, my scale could not keep up with me. On that day in August, when I hit the 300 lbs., I stepped on the scale and looked down to see my weight. The scale beeped and displayed the following: OVER LIMIT. That incident was not enough to make me change my behavior. Rather than work to lose weight, I bought an old fashion medical scale that went up to 400 lbs. (Warning Sign Ignored)

Years ago, I bought a top-of-the-line treadmill. I never thought that I would have to worry about weight-limits. I had no idea that the treadmill had a maximum weight capacity of 275 lbs. Several years later I got on the treadmill, and it reflected a digital readout that told me I was over the weight limit to use it. I ignored that warning and continued to use the treadmill. A few months later, I was walking on the treadmill and started to smell smoke. I burned the motor on the treadmill, and it shut down. You would think that incident would have been enough to make me change my lifestyle. Nope. I did not change my behavior and continued to gain weight eventually reaching 350 lbs. (Warning Sign Ignored)

And Then This Happened
In 2021, I was experiencing occasional heart racing while sitting at my desk or laying down. One of my buddies who had heart surgery DEMANDED that I visit my doctor ASAP. My doctor referred me to a cardiologist. Long story short, between the time of the thermonuclear tests at the hospital and the time to get the results, I was expecting bad news, but I was optimistic that I would be OK. Without getting too deep, the doctor sat me down and said: “You have a blockage on the left side of your heart. We will not be operating on you. Your heart has done what we call a WAZE, like the GPS system and re-routed enough blood to your heart.” WOW! About 20-months later, another blockage was detected on the right side of my heart. Again, no surgery required. I will end the story there by saying: “God is good!”
The Pivotal Moment
And then one day, I had a S.E.E. moment. I was watching my friend and colleague Marc DeSimone on stage teaching a group of managers. We used to watch each other when were booked together by the client. One day Marc spoke about S.E.E., which stands for Significant Emotional Event. The S.E.E. moment that rocked me to the core and put me on track to lose 68 lbs. happened in 2022 while traveling with friends and family. We boarded an airplane and were about to take off. The Flight Attendant was walking down the aisle to ensure that everyone had their seatbelt fastened. There I sat, sweat pouring down my brow trying to get my seatbelt to click. The Flight Attendant saw me struggling and announced rather loudly, “Looks like you’re going to need a seatbelt extender.” I was devastated, embarrassed and humiliated. I looked up at the Flight Attendant. I wanted to say, “Why don’t you get on the P.A. system and tell everybody.” I was too fat for the seatbelt.

That was my S.E.E. moment. I immediately began to reflect on my circumstances. I had to figure out how I got to this point. If I could figure that out and honestly deal with the answers, I believe I would have a chance.
Take Baby Steps Along the Way
My first step to success was intermittent fasting. That was my first measure of success, and it made me feel good. From this point on, I believed that losing weight and keeping it off was possible. I also had CONFIDENCE and was comfortable holding myself accountable. I asked myself: “What might I be doing that could be contributing to my repeated setbacks and subsequent weight gain?” I also had to make myself vulnerable and trust that those folks around me were giving me feedback from a “good place” with “good intentions.” I simply had to accept their feedback. Once that happened, I was able to successfully manage this process of living a healthier lifestyle and losing weight.
I won’t make this post any longer, but as you can see, I figured it out. One of the things I did back then was visit the website “Chubby Travelers.” This site is designed for overweight people. They rank airlines, review airline seats (pitch and width), seatbelt extenders, buses and anything that a fat person would need or should know when traveling.

Bottom Line: To those who reached out to me to thank me for my last post, hang in there. You are not alone, and you can do it!

Gary Johnson is the Founder and Publisher of Black Men In America.com, an online news and magazine, Black Boating and Yachting.com and several other online sites. Gary is also the author of the book “25 Things That Really Matter In Life,”: A Quick and Comprehensive Guide To Making Your Life Better—Today!, and a contribution author to “The Black Father Perspective: What We Want America To Know,” and “In Search of Fatherhood – Transcending Boundaries: International Conversations on Fatherhood.“
Posted July 23, 2024
Tips for Protecting Your Eyes as a Black American with Diabetes

According to the Centers for Disease Control’s (CDC) National Diabetes Statistics Report for 2022, cases of diabetes have risen to an estimated 37.3 million across the US. While diabetes impacts people of all social and economic backgrounds, there are disparities across racial and ethnic groups. More specifically, the risk of developing diabetes is 77% greater among African Americans. Limited access to healthcare, higher rates of obesity, and the prevalence of hypertension contribute to this increased risk.
For those already diagnosed with diabetes, it is essential to pay close attention to eye health. Diabetes can have serious implications for vision, leading to conditions that may result in blindness if left untreated. In this article, we’ll explore how diabetes affects eye health and provide practical tips to help individuals protect their vision.
How diabetes impacts eye health
Did you know that diabetes is the primary cause of blindness in adults ages 20 to 74? The National Institutes of Health states that diabetes mainly affects the eyes when blood glucose (blood sugar) is too high. In the short term, this may manifest in blurry vision caused by high glucose, which leads to swelling in the tissues of the eyes. However, over time, more serious eye conditions may develop due to blood vessel damage.
Diabetic eye diseases include diabetic retinopathy, cataracts, and glaucoma – all of which may result in poor vision or even blindness. Although diabetic retinopathy is the most common cause of vision loss among diabetic patients, having diabetes makes you two to five times more likely to develop cataracts. Meanwhile, diabetes doubles the risk of glaucoma.
Managing your diabetes can help you prevent or delay vision loss, but there are also proactive steps you can take to maintain eye health.
Tips for preventing vision issues from diabetes
Protect your eyes from UV rays
Ultraviolet (UV) rays from the sun can exacerbate eye problems for people with diabetes. For instance, prolonged exposure to UV light increases the risk of cataracts and other eye conditions. Therefore, wearing sunglasses that block 100% of UV rays is crucial. In addition, Dr. Jessica S. Watson recommends opting for sunglasses with oversized frames to maximize eye coverage and reduce UV absorption, such as the Oakley Holbrook or Ray-Ban Balorama. To further shield your eyes from harmful rays, you can wear a wide-brimmed hat like the UV Protection Wide Brim Hat from Uniqlo.
Regularly update your prescription glasses
Diabetes can cause fluctuations in blood sugar levels that trigger changes in vision. Prescription updates, coupled with regular eye exams, ensure you have the correct lenses to support your vision needs. The good news is that established online retailers have simplified this process. Leading eyewear brand Ray-Ban offers a range of high-quality eyeglasses to suit various needs, from single-vision to progressive and even photochromic lenses. Simply manually enter your prescription, upload a file, or send an email or text to customize glasses with your prescription. Best of all, this retailer accepts most major insurance networks and requires just a few details to identify your eligibility.
Undergo diabetic eye exams
Having a full, dilated eye exam is the best way to check for eye problems from diabetes. These comprehensive eye exams include tests that specifically look for signs of diabetic retinopathy, glaucoma, and cataracts. Early detection through these exams allows for timely intervention, preventing or slowing the progression of eye diseases. Experts advise that individuals with diabetes have a dilated eye exam at least once a year. During this exam, your eye doctor will dilate your pupils with special eye drops to get a better view of the inside of your eyes. This thorough examination helps in identifying any changes or damage caused by diabetes.
Protecting your vision is a crucial aspect of managing diabetes, particularly for African Americans who face a higher risk of developing the disease. By understanding the impact of diabetes on eye health and following these practical tips, you can take preventive measures to preserve your vision.
Article written by Rose Henderson exclusively for Black Men In America.com
Photo Credit: https://www.freepik.com/free-photo/doctor-patient-ophthalmologist-s-office_78551137.htm
![]()
Posted July 17, 2024
Cultivate Mindfulness and Reap Contentment Daily

In today’s fast-paced world, finding calm moments can seem challenging. However, integrating mindfulness into your daily life can be a powerful way to enhance your well-being.
This article from BlackMenInAmerican.com explores practical strategies for fostering mindfulness, emphasizing simple yet impactful practices. Without delving into the specifics just yet, let’s embark on a journey to discover how these techniques can transform your everyday experiences.
Unplugging for Presence
Regular periods of disconnection from electronic devices are crucial. This practice fosters a deeper connection with oneself and the surrounding environment, paving the way for a more mindful existence.
By setting aside time each day to step away from screens, individuals can foster an environment conducive to mindfulness, allowing for an enhanced awareness of the present moment. This deliberate pause from the digital world helps cultivate a space where one can reconnect with one’s thoughts and feelings, encouraging a serene state of mind.
The Art of Gratitude
Cultivating a gratitude journal encourages reflection on the positive aspects of life, big and small. This act of appreciation enhances your ability to live in the moment and view challenges as opportunities. Writing down what you’re thankful for each day shifts the focus from what’s lacking to what’s abundant in life, which fosters a positive mindset. This practice promotes mindfulness and contributes to overall happiness and well-being, illustrating gratitude’s transformative power.
Movement and Mindfulness
Incorporating gentle exercises such as yoga or tai chi into your routine can significantly enhance physical and mental well-being. These activities promote a harmonious balance between body and mind. By engaging in movements that require attention and breath control, individuals can cultivate a state of mindfulness that transcends the exercise itself. This integration of movement and mindfulness nurtures a deeper awareness of the body and its sensations, leading to increased mental clarity and stress reduction.
Discovering Inner Stillness
Engaging in body scan meditation allows for a profound connection with one’s physical self, encouraging relaxation and mindfulness. This practice involves mentally scanning your body for areas of tension and consciously releasing it, fostering a heightened state of body awareness. Such meditation not only aids in relaxation but also promotes a mindful acknowledgment of one’s physical presence, offering a pathway to inner peace amidst the hustle and bustle of daily life.
Journaling with Video
Incorporating video journaling into your self-care routine can provide a unique and dynamic way to express emotions, track personal growth, and reflect on your thoughts over time. Using a video creator, you can capture a more intimate and authentic form of self-expression compared to written journaling, capturing nuances in your mood and body language. This practice not only enhances self-awareness but also serves as a powerful tool for visualizing progress and fostering a deeper connection with yourself.
Mindful Eating
Embrace the practice of eating slowly and without distractions. This approach to meals nurtures a deep appreciation for food and its nourishment, enhancing the dining experience. By focusing on the flavors, textures, and aromas of what you eat, you cultivate a mindful relationship with food. This attentiveness not only improves digestion but also encourages a more enjoyable and satisfying eating experience, highlighting the significance of mindfulness in everyday activities.
Breathing with Purpose
Dedicate time each day to focus solely on your breath. This simple practice can serve as a powerful tool for centering and calming the mind. By concentrating on the rhythm of your breath, you can anchor yourself in the present moment, effectively reducing stress and anxiety. This practice of mindful breathing serves as a foundation for mindfulness, demonstrating that even the most basic actions can have a profound impact on mental well-being.
Listening to Understand
Make a conscious effort to listen to others without immediately responding. This form of active listening fosters deeper, more meaningful connections. By fully engaging with the speaker, you not only enhance your understanding of their perspective but also cultivate a sense of presence and mindfulness in your interactions. This approach to communication enriches relationships and promotes a more mindful way of engaging with the world.
Incorporating mindfulness into your daily routine doesn’t require drastic changes. Through small, intentional actions, you can significantly enhance your quality of life. By adopting these practices, you’ll discover the profound impact of living in the present, cultivating a deeper sense of peace and contentment. Embrace these strategies as a pathway to a more mindful, fulfilling existence.
For current events and political analysis focused on black men, visit BlackMenInAmerica.com.
Disclaimer: This page and other portions of this website and podcast that offer health, fitness and nutritional information is designed for educational purposes. You should not rely on this information as a substitute for, nor does it replace, professional medical advice, diagnosis, or treatment. If you have any concerns or questions about your health, you should always consult with a physician or health care professional. Do not disregard, avoid or delay obtaining medical or health related advice from your health-care professional because of something you may have read on this site. The use of any information provided on this site is solely at your own risk. Developments in medical research may impact the health, fitness and nutritional advice that appears here. No assurance can be given that the advice contained in this site will always include the most recent findings or developments with respect to the particular material.
![]()
Addressing Obesity and Its Comorbidities among the Black Community

By Rose Henderson Exclusively for Black Men In America.com
It’s no secret that an obesity epidemic is ravaging the United States. As of 2024, nearly 43% of American adults are obese. Unfortunately, while obesity is present in all demographics, data reveals that the Black community is disproportionately affected. More recently, studies have found that incidences of obesity in the Black population are more common than in other ethnic groups, regardless of a person’s socioeconomic status. On average, Black women are 57% more likely to become obese than women of other races, while Black men are about 41% more likely. Given that obesity is a chronic condition that can trigger and worsen numerous ailments, it’s important to understand how it impacts the Black community and the specific comorbidities it may bring.
Understanding obesity and its roots in the Black community
Contrary to popular belief, obesity is not just a reflection of a person’s diet and exercise. Nor is it an interchangeable term with simply being overweight. For starters, when studying the difference between overweight and obese individuals, there is a distinct difference in the body mass index (BMI). While those who are overweight have a BMI between 25 and 29.9, those who are obese have a BMI of 30 and above. Potentially, some people confuse the two because being overweight is also called “pre-obesity.”
As mentioned above, another important point about obesity that has to be understood is that it is brought on by multiple complex factors. While food and activity levels do play a part, most people’s obesity is also shaped by factors that are harder to control, like genetics, sleep quality, and family history. In line with this, obesity in predominantly African-American neighborhoods has historically been attributed to the lack of health resources, fitness initiatives, and balanced food sources. The same Wiley study cited above also reveals that Black people are also subject to cultural body image pressures that perpetuate obesity as normal or inevitable. Sadly, evidence suggests that Black communities are not just more prone to obesity, but they’re also more vulnerable to more significant comorbidities. Here are some of the most notable obesity comorbidities among the Black populace.
Obesity comorbidities Black men and women are at risk of Cancer
According to studies, obesity causes a person to have more fat tissues and fat cells. These are known to influence hormone levels, which, over time, can lead to increased cell production. As per the National Cancer Institute, this can encourage the growth of tumors or the development of certain cancers. These include ones common in the Black community, like prostate cancer. The Prostate Cancer Foundation (PCF) explains that Black men tend to be diagnosed with an aggressive form of this cancer at an earlier age than their peers. Along the same lines, obesity can also put people at more risk of stomach cancer, which both Black men and women are twice as prone to.
Stroke
Compared to their White and Hispanic counterparts, Black adults are up to 70% more likely to succumb to a stroke. While strokes are more common in people over the age of 65, obesity heightens the risk of this happening at any age. Furthermore, obesity increases the chances of having a stroke by 64%. The reason why obesity can cause a stroke is because excess weight can contribute to blood pressure, which can lead to blood clots in the brain. Also, having a chronically high body weight can result in metabolic syndrome, where a person has elevated cholesterol, blood sugar, and triglycerides. These have been found to damage blood vessels, which, over time, can make clots more possible.
Diabetes
Over the last three decades, researchers have found that racial disparities now see Black adults have a 50% higher chance of developing Type 2 diabetes. Diabetes and obesity are linked because of the more pronounced abdominal and intra-abdominal fats. This has been found to cause insulin resistance. In the long run, being diabetic can make it difficult to lose weight, which can make it harder to get fit and healthy.
Watch our Health & Wellness Videos Below

Start Your Recovery.org Local Treatment and Resources in Los Angeles
Credit: YAKOBCHUK VIACHESLAV / Shutterstock
The Food and Drug Administration’s (FDA) suggestions for avoiding a protein deficiency are a lot lower than what the average, visibly muscular person will tell you they eat. Avoiding a deficiency is a lot different than growing muscle mass. To sort through all these murky waters, we talked to multiple experts and look at a ton of research to land on the formulas used in our protein intake calculator.
- How Does Protein Help Muscles Grow?
- Benefits of Protein
- What’s a High Quality Protein?
- How to Track Your Protein Intake
- How Much Protein Should I Eat at Once?
- Protein Intake Calculator
- How We Calculated Your Protein Intake
- Frequently Asked Questions
Editor’s Note: The content on BarBend is meant to be informative in nature, but it shouldn’t take the place of advice and/or supervision from a medical professional. The opinions and articles on this site are not intended for use as diagnosis, prevention, and/or treatment of health problems. Speak with your physician if you have any concerns. Read the full article here.
![]()
Health and Mental health Resources
National Alliance on Mental Health
Black Emotional and Mental Health Collective (BEAM)
Group aimed at removing the barriers that Black people experience getting access to or staying connected with emotional health care and healing through education, training, advocacy and the creative arts.
Black Men Heal
Limited and selective free mental health service opportunities for Black men.
Black Mental Health Alliance — (410) 338-2642
Provides information, resources and a “Find a Therapist” locator to connect with a culturally competent mental health professional.
Black Mental Wellness
Provides access to evidence-based information and resources about mental health and behavioral health topics from a Black perspective, as well as training opportunities for students and professionals.
Black Women’s Health Imperative
Organization advancing health equity and social justice for Black women through policy, advocacy, education, research and leadership development.
Boris Lawrence Henson Foundation
BLHF has launched the COVID-19 Free Virtual Therapy Support Campaign to raise money for mental health services provided by licensed clinicians in our network. Individuals with life-changing stressors and anxiety related to the coronavirus will have the cost for up to five (5) individual sessions defrayed on a first come, first serve basis until all funds are committed or exhausted.
Brother You’re on My Mind
An initiative launched by Omega Psi Phi Fraternity, Inc. and NIMHD to raise awareness of the mental health challenges associated with depression and stress that affect Black men and families. Website offers an online toolkit that provides Omega Psi Phi Fraternity chapters with the materials needed to educate fellow fraternity brothers and community members on depression and stress in Black men.
Ebony’s Mental Health Resources by State
List of Black-owned and focused mental health resources by state as compiled by Ebony magazine.
Melanin and Mental Health
Connects individuals with culturally competent clinicians committed to serving the mental health needs of Black & Latinx/Hispanic communities. Promotes the growth and healing of diverse communities through its website, online directory and events.
Mocha Health
Online community for Black women to seek support.
Ourselves Black
Provides information on promoting mental health and developing positive coping mechanisms through a podcast, online magazine and online discussion groups.
POC Online Classroom
Contains readings on the importance of self care, mental health care, and healing for people of color and within activist movements.
Sista Afya
Organization that provides mental wellness education, resource connection and community support for Black women.
Therapy for Black Girls
Online space dedicated to encouraging the mental wellness of Black women and girls. Offers listing of mental health professionals across the country who provide high quality, culturally competent services to Black women and girls, an informational podcast and an online support community.
The SIWE Project
Non-profit dedicated to promoting mental health awareness throughout the global Black community.
The Steve Fund
Organization focused on supporting the mental health and emotional well-being of young people of color.
Self-Care for People of Color
We recognize that many mental health conditions are being triggered as a result of the coronavirus, the economic crisis and repeated racist incidents and death.
Learn more about mental health conditions including anxiety disorders, depression and post-traumatic stress disorder.
- Coping with anticipatory grief
- Coping with traumatic stress
- Read about Racial Battle Fatigue
Treatment Directories
- Association of Black Psychologists Directory
- Inclusive Therapists
- Innopsych
- LGBTQ Psychotherapists of Color Directory
- National Queer and Trans Therapists of Color Network
- Psychology Today Directory of African American Therapists
- Therapy for Black Men
Educational Resources on Racism And Inequality
Understanding the context of racism and recent events
- Video on understanding racism and the reactions to the death of George Floyd and many others
- Video on understanding the perspectives of your colleagues of color
- Article on “White Privilege: Unpacking the Invisible Knapsack”
- List of Anti-Racism resources
Understanding the context of racial inequality that impacts mental health
- APA Best Practices on working with Black patients
- APA Mental Health Facts for Black Americans (2017)
Understanding and addressing the social determinants of health that impact mental health
- Article on improving the health of Black Americans and the overdue opportunity for social justice
- Video on understanding the social determinants of health and toxic stress
- Video on the social determinants of toxic stress, specifically race and ethnic toxic stress
- APA Stress & Trauma Toolkit for treating Black Americans in a changing political and social environment
- The Robert Wood Johnson Foundation Page on Achieving Health Equity — Information about why health equity matters and what you can do to help give everyone a fair shot at being as healthy as they can be.
Ways to Take Action as An Ally or Champion for People of Color
- Article on being a white ally through word, actions and power
- Article on being a white ally for racial justice
- Community based organizations to partner with: Color of Change, Black Lives Matter, Campaign Zero, Innocence Project
Books to Read
- Eloquent Rage: A Black Feminist Discovers Her Superpower by Dr. Brittney Cooper
- Me and White Supremacy by Layla F. Saad
- So You Want to Talk About Race by Ijeoma Oluo
- How To Be An Antiracist by Dr. Ibram X. Kendi
- The Fire Next Time by James Baldwin
- The New Jim Crow: Mass Incarceration in the Age of Colorblindness by Michelle Alexander
- The Next American Revolution: Sustainable Activism for the Twenty-First Century by Grace Lee Boggs
- The Warmth of Other Suns by Isabel Wilkerson
- White Fragility: Why It’s So Hard for White People to Talk About Racism by Robin DiAngelo, PhD
- When Affirmative Action Was White: An Untold History of Racial Inequality in Twentieth-Century America by Ira Katznelson
Source: National Alliance on Mental Illness
StartYourRecovery.org encourages people to find the support they need, or to help their loved ones encourage and support help-seeking. We hope this website is an easy way to learn about substance use and addiction and to determine your next step, whether it’s having a conversation, learning more, or seeking professional help.
While they cannot diagnose or treat substance use and mental health conditions, they can say with confidence: Help is available, and treatment works.
Click here to hear stories from people who have dealt with addiction and from their family members and friends who lent their support.
Alcohol Rehab Help
In This Article
What are Benzodiazepines?
Benzodiazepines (benzos) are prescription medications that treat mood disorders, anxiety, and panic attacks. They can also be used as muscle relaxers. Benzos are effective and safe when used correctly. However, the medications are very addictive.
If someone takes benzodiazepines in high doses, tolerance develops over time. The body is used to taking the drugs and needs them to function normally. Withdrawal occurs if use is stopped abruptly, and these symptoms can be life-threatening.
Benzodiazepine Uses
In addition to treating anxiety and panic attacks, benzodiazepines can also treat:
- Depression
- Insomnia
- Seizures
- Nausea and vomiting
- Muscle tension
How Do Benzodiazepines Work?
Benzodiazepines act as sedatives, which means they slow down the body’s functions. The drugs work by increasing the effect of GABA (gamma-aminobutyric acid), a chemical in the brain. GABA reduces activity in the areas of the brain responsible for rational thought.
GABA is considered an inhibitory neurotransmitter because it decreases activity in your nervous system by blocking certain brain signals. When GABA attaches to a specific protein in your brain (the GABA receptor), a calming effect is produced. This relaxing effect reduces feelings of stress, fear, and anxiety. This is why benzodiazepines are so effective (and extremely addictive).
Side effects of benzodiazepine use can include:
- Drowsiness
- Confusion
- Memory issues
- Speech problems
- Blurry vision
- Dry mouth
- Muscle weakness
- Unsteadiness
- Headaches
- Constipation
- Nausea and flu-like symptoms
- Light-headedness and dizziness
Addiction Treatment for Drugs or Alcohol
Find Help For Addiction Issues. Find The Support You Need To Get Clean. Call now (855) 217-2693
Medical Detox Program
Whether you’ve become addicted to prescription medications, street drugs, alcohol or a combination of substances, medically supervised detox is a specialized inpatient program that is designed to help you through the physical withdrawal process. Our team of licensed, experienced detox experts provide 24/7 care that includes a comprehensive medical assessment and ongoing management of your withdrawal symptoms in a safe, comfortable environment.
Don’t let fears over the detox process keep you from taking control of your life. Getting clean and sober is a critical step in your long-term recovery journey, and we’re here to provide you with the support, guidance and expert medical care you need to detox safely.
Click Here For More Information
Want to Learn More? Dial: 1-844-861-7743
As the Chief Visionary of The JLJ Foundation, Mrs. Jones suffers from not just one chronic illness, but three. She lives with Epilepsy, Lupus, and Diabetes, and each of those illnesses allows for her to be a support system to others living with a chronic illness.
She has volunteered with the National Office of the Epilepsy Foundation of America, as well as participated in the National Walk for Epilepsy. Currently, she is a certified fitness and nutrition coach. She is also a devoted wife and mother.
Check out our exclusive interview with Jaimi Jones.

 Left to Right: Photo #1 Jaimi Jones Lifting, Photo 2: Jaimi and Gary Johnson (March 2018)
Left to Right: Photo #1 Jaimi Jones Lifting, Photo 2: Jaimi and Gary Johnson (March 2018)
To learn more about Jaimi click here to visit her official website.
Is Fast Food Healthier When It’s Plant-Based?
Alternatives to animal products aren’t necessarily better for you
In November 2020, McDonald’s announced plans to roll out plant-based versions of its signature items, including a burger, chicken sandwich, and breakfast sandwich made with plant-based sausage. The new menu, called the McPlant, is hardly a surprise.
McDonald’s is a latecomer to the plant-based fast-food game: White Castle debuted the Impossible Slider in April 2018. Shortly after, Del Taco and Burger King added Beyond and Impossible products to their menus, respectively. Then Dunkin’ released a breakfast sandwich made with plant-based sausage, and KFC and Jack in the Box began rolling out meatless chicken in select markets. These options, part of a massive innovation boom in alternative meat, are engineered to be extremely similar to the meats they mimic. They’re different from old-school veggie burgers, which were just plant proteins like beans or soy in the shape of a small patty. These new products are still made from a mishmash of plant proteins, but they look, smell, cook, and taste like the real deal.
As a nutrition journalist, I find the whole trend a little baffling. The number of Americans who follow a vegetarian diet hasn’t changed much in recent decades. In fact, adult vegetarians in the U.S. dropped from 6 percent of the population to 5 percent between 1999 and 2019, according to a Gallup poll. And while many vegetarians are OK eating food cooked with the same griddles and deep fryers as meat, those who aren’t have voiced concern over the cross contamination that happens at certain fast-food joints. (Many chains include a disclaimer on their website as well as their menu stating that this is the case, so it’s worth looking into or asking a staff member about if this is a deal breaker for you.) Still, vegan and vegetarian options are trending like never before, likely because more customers are interested in eating sustainably.
The number of American adults concerned about climate change is growing dramatically, up from 44 percent in 2009 to 60 percent in 2020, according to the Pew Research Center. And 55 percent of respondents in a 2020 Yale University survey reported that they are willing to eat less meat as a way to combat it. If you’re a major fast-food company, that’s a trend worth capitalizing on.
The term “plant-based” often gets an automatic health halo: it reads as synonymous with “good for you,” no matter the context. And when done right, it can be. A 2016 review found that plant-based diets were linked to a lower risk of heart disease and diabetes, because they’re generally low in saturated fat, high in fiber, and nutrient dense. But that’s an entire diet they’re talking about, not a single ingredient or meal. And these new plant-based meats are popular because they are engineered to be as close to the real deal as possible—not just in taste and texture but nutritionally, too.
Both Beyond and Impossible burgers contain 20 grams of protein per four ounces, while the same amount of 85 percent lean ground beef has 21 grams. The plant-based protein comes from a variety of sources—rice, pea, and mung bean protein in Beyond beef; soy and potato protein in Impossible beef. Since protein is important for both performance and general health, the fact that you can get just as much of it from plant-based beef as regular beef is a good thing.
But there are downsides. Impossible beef contains the same amount of saturated fat as 85 percent lean ground beef: eight grams per four ounces. Beyond recently lowered its saturated fat content, but a serving still contains five grams. The Dietary Guidelines for Americans recommend limiting saturated fat to less than 10 percent of your total calorie intake, or about 22 grams per day for someone who eats around 2,000 calories. Too much saturated fat is associated with an increased risk of heart disease and stroke, regardless of whether it comes from plants or animals.
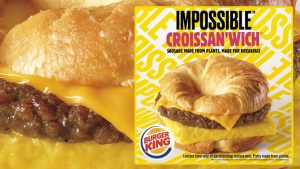 Destini Moody, a dietitian and athletic trainer based in San Francisco, points out that plant-based meat also tends to be higher in sodium than regular meat. The Impossible Whopper has about 10 percent more sodium than its beef counterpart. Even before cooking or seasoning, beef from both Beyond and Impossible has more than 350 milligrams of sodium per four ounces, compared to 75 milligrams in 85 percent lean ground beef. The Dietary Guidelines for Americans recommend consuming less than 2,300 milligrams of sodium per day, since too much can contribute to high blood pressure, increasing your risk of heart attack and stroke. “I can’t say that plant-based burgers are a healthier choice than just getting a regular beef burger,” Moody says.
Destini Moody, a dietitian and athletic trainer based in San Francisco, points out that plant-based meat also tends to be higher in sodium than regular meat. The Impossible Whopper has about 10 percent more sodium than its beef counterpart. Even before cooking or seasoning, beef from both Beyond and Impossible has more than 350 milligrams of sodium per four ounces, compared to 75 milligrams in 85 percent lean ground beef. The Dietary Guidelines for Americans recommend consuming less than 2,300 milligrams of sodium per day, since too much can contribute to high blood pressure, increasing your risk of heart attack and stroke. “I can’t say that plant-based burgers are a healthier choice than just getting a regular beef burger,” Moody says.
When it comes to plant-based chicken versus the real thing, Moody explains that it’s likely the same story, since both are breaded and fried. KFC doesn’t list the nutrition information for Beyond Fried Chicken on its website (which is a little odd, as the company lists it for everything else), but according to Prevention, one nugget has 60 calories, one and a half grams of saturated fat, and five grams of protein. It’s hard to compare that to its regular chicken, since KFC doesn’t have chicken nuggets. But one extra-crispy chicken tender (the closest thing on the menu to Beyond Fried Chicken) has 260 calories, two grams of saturated fat, and 19 grams of protein per serving. That means that, per calorie, the plant-based nuggets actually have less protein and more saturated fat than regular chicken tenders.
Sustainability—and Accessibility—Count
It’s not all bad news. If your main concern is planetary health, plant-based foods are the better choice. Yes, some of the research touting the sustainability of plant-based meat is funded by the same companies that make it, which might overestimate its positive impact. But experts agree that plant-based foods have a smaller environmental impact than animal products, processed or not.
A May 2020 article published in the journal Global Environmental Change looked at data from 140 countries and concluded that a vegan diet has a 70 percent smaller carbon footprint than a traditional diet. Animal products require a lot of resources: about 77 percent of the habitable land on earth is used to raise livestock or grow livestock feed, but those animals make up just 18 percent of the calories produced for human consumption. In order to sustainably feed the growing number of people on the planet, we have to adjust the way we eat.
Plant-based options at fast-food restaurants that actually taste good might help get more people on board with a planet-friendly diet. “Corporations are providing these offerings not only for vegans and vegetarians but for meat-eating customers who are interested in plant-based options as well,” says Taylor Wolfram, a Chicago-based dietitian who specializes in veganism. She points out that Burger King had another veggie burger on its menu for years, but it didn’t taste anything like beef and only existed on the menu so that there was a vegetarian option. “Now that there are beef-like alternatives, I think a lot more meat eaters are going for these options,” Wolfram says. She’s right—MarketWatch reported on a survey showing that 95 percent of people who bought these new plant-based burgers in 2019 were meat eaters.
Impossible Whoppers and McPlant sandwiches also make plant-based eating more accessible to those who rely on fast food for many of their meals, whether that’s due to convenience, price, or preference. On any given day, 36 percent of American adults eat fast food, according to a 2018 report from the Centers for Disease Control and Prevention. If even a fraction of those 85 million Americans went plant-based for their meal, it could have a significant environmental impact. While these new alternatives typically cost between one and two dollars more than their meat-based counterparts, Wolfram still thinks that they could have a broad enough appeal to create change. If that Impossible Whopper convinces a diehard carnivore to give plant-based options a chance, then that’s certainly something.
It’s Still Fast Food
If you eat fast food often and want to lessen your carbon footprint, plant-based menu items are a good choice. But if you only eat it occasionally, just go ahead and order what you’re craving. Whether they’re made from plants or animals, the menu items at your local McDonald’s aren’t terribly nutritious. And that’s OK. No single food will make or break your diet, and you don’t need to choose the healthiest option every time you eat. A good diet means you’re getting the nutrients your body needs, but it also means you’re eating what you want. Maybe that’s an Impossible Whopper, and maybe it’s a Big Mac.
This article was originally published in Outside Online.com on February 3, 2021 and written by Christine Byrne, a food and health writer who hopes to make wellness more accessible (and fun!) for everyone. Previously, she was the features editor at Self, and the food editor at BuzzFeed. She lives in North Carolina and is working toward a Master’s in public health with a nutrition concentration.
For additional plant-based resources check out the following books.
Check out and support the website soulPhoodie
Why Are African Americans At A Higher Risk Of Contracting Deep Vein Thrombosis?
Contribution by Sally Writes
As many as 100,000 deaths occur in the U.S. every year because of deep vein thrombosis (DVT) – a condition that occurs when a blood clot forms in a vein, usually in the leg area. DVT can be dangerous and even fatal. The Office of Minority Health at the Department of Health and Human Services has warned that African-Americans are at a much higher risk for this condition than people of other ethnic backgrounds. The risk is particularly high following serious illness, surgery or other types of trauma. If you are worried about DVT, what signs should you watch out for, and how can you reduce your risk factors?
Reducing Your Likelihood Of Developing DVT
The first steps for African Americans wishing to lower their chances of developing DVT is to look at additional factors that can further raise their risk. These include being overweight, smoking, being on contraception or Hormone Replacement Therapy, having cancer or heart failure, and having varicose veins. Situational risks can also exist. These include taking a long plane or car ride (sitting in one position for a long time) and leading a sedentary lifestyle. For all these reasons, following a healthy diet and taking daily exercise are important. Even if you do have a desk job, you can battle DVT by getting up every hour to stretch, run up and down steps, or simply take a short brisk walk. Remember that doing half an hour of exercise as recommended by doctors may not be enough if you sit down for several hours straight.
What Symptoms Should You Watch Out for?
Symptoms of DVT are varied and can include leg pain, swelling, feverish skin, red or patchy skin, and coughing up bloody mucus. DVT symptoms should be considered a medical emergency. The overall prevalence of DVT is up to 60% higher in black men and women (this is true regardless of gender) and black people also have a higher rate of pulmonary embolism and pregnancy-associated DVT than other groups.
Why Do More Black People Have DVT?
Despite various studies into the subject, scientists are still unable to fully define potential reasons for interracial differences in DVT risks between black Americans and other groups. One postulation is that the inheritance of hemoglobin S (a particular kind of protein in blood cells that is found in sickle cell disease) may increase the risk of thrombosis. As reported in a case study by T Buckner et al, sickle cell trait is found in up to 8% of black Americans, and people with sickle cell disease have an “overactive coagulation system.” More black Americans also have specific conditions that may be related to an elevated DVT risk. These conditions include hypertension, diabetes mellitus, and chronic kidney disease. Finally, black Americans have high levels of two important clotting proteins that can lead to increased coagulation.
Black Americans (both men and women) have a higher risk of DVT than other members of the American population. Risk factors for this condition are known – they include hypertension and sedentarism, for instance. To reduce your risk of developing DVT, stay at a healthy weight, consume a healthy Mediterranean-style diet, and keep active as recommended by your doctor.
How Can Medications Negatively Impact Your Oral Health?
By Alyssa Hill – New Mouth.com
Prescription and over-the-counter medications can negatively impact your general and oral health. In particular, common complications associated with everyday medications include irregular bleeding, changes in taste, soft-tissue reactions (sores), dry mouth, and enlarged gum tissue.
During routine dentist appointments, it is important to tell them which medications you are taking to ensure you receive the best care possible. In addition, if you currently have any chronic conditions or illnesses, let your dentist know before or during your next appointment.
Common Oral Complications Associated with Medications
Dry mouth, gum inflammation, mouth sores, cavities, and oral thrush are common conditions associated with many everyday medications. Some of these diseases are harmless, while others can be indicators of more serious health conditions.
Common oral conditions that may arise while taking certain medications include:
Dry Mouth
Medication-induced dry mouth is an uncomfortable side effect that impacts many older adults. By definition, dry mouth (xerostomia) is an oral condition when the salivary glands in the mouth do not produce enough saliva to keep the mouth wet.
Saliva is essential for cavity protection because it repairs tooth enamel through remineralization and washes out plaque bacteria. However, as the production of saliva decreases, oral dryness is more likely to occur, which can result in decay or tooth loss.
Untreated dry mouth can lead to bad breath, gum disease, and painful mouth sores. It can also cause dental erosion, which is a chemical process that results in the loss of dental tissue.
There are thousands of everyday medications that can cause dry mouth. Although, the most common prescriptions that may result in xerostomia include the following:
- Antidepressants — most types of antidepressants are used to treat depression. In particular, popular antidepressants include Celexa, Wellbutrin, Paxil, Prozac, and Savella.
- Muscle Relaxers — these medications treat muscle spasms and discomfort. Popular muscle relaxants include Robaxin, Somas, and Flexeril.
- Decongestants — these over-the-counter medications reduce allergy symptoms. Common brands of decongestants include Afrin, Sudafed, and Vicks.
- Diuretics — diuretics are also called “water pills.” They are commonly used to help treat high blood pressure.
- Antihistamines — medications that stop allergy symptoms, including hay fever, flu symptoms, and food allergies.
- Appetite Suppressants — these over-the-counter medications (vitamins) reduce appetite, thus decreasing food consumption.
- Blood Pressure Medications — this includes diuretics, beta-blockers, alpha-blockers, and calcium channel blockers, among others.
Soft-Tissue & Gum Reactions
Certain prescription medications are linked to mouth sores, tissue discoloration, and inflammation. So, if you experience soft-tissue inflammation after taking any of these pills, contact your dentist immediately. He or she can then create a custom oral hygiene regimen to help decrease discomfort and symptoms. Medications that may cause oral ulcers and/or inflammation in the mouth include the following:
- Blood Pressure Control Medications — these medications include diuretics, beta-blockers, alpha-blockers, and calcium channel blockers, among others.
- Immunosuppressive Agents — drugs that suppress the immune system and decrease the rejection of transplant organs.
- Oral Contraceptives — birth control pills contain estrogen and progestin, which can increase inflammation in the body.
- Chemotherapy — chemo treatment can result in oral health complications, including soft-tissue reactions in the mouth. Dry mouth is also common.
Further, other types of prescription medications can cause enlarged gum tissue (gingival hyperplasia). Gum tissue overgrowth occurs when the gums become inflamed and discolored. This condition is typically a symptom of gum disease and poor oral hygiene. Certain medications can also cause gingival hyperplasia, including:
- Phenytoin — slows down and reduces seizures.
- Immunosuppressant Drugs — drugs that prevent immune system activity.
- Calcium Channel Blockers — these drugs are commonly prescribed to people with blood pressure issues.
- Heart Medications — medications taken for heart disease or high blood pressure can cause soft-tissue reactions in the mouth.
Oral Thrush
Oral thrush (oral candidiasis) is a yeast infection that forms due to the overgrowth of Candida fungus that lives in the mucous membranes lining in the mouth. Most people have small traces of Candida in their mouths. For some, the fungi can overgrow and cause thrush. However, if you have a strong immune system, the fungus does not overgrow.
The most common sign of thrush is white spots (lesions) that wipe off and leave a red, raw base. These lesions can also develop on the palate, tongue, lining of the cheeks, or back of the lips.
If you are taking medications that increase your risk for dry mouth, oral thrush can develop over time. Other medications that can also cause thrush include:
- Inhaled Steroids — these steroids are prescribed to people with asthma (e.g. inhalers).
- Certain Antibiotics — penicillins, cephalosporins, and tetracyclines can cause oral candidiasis.
- Prednisone — medications that treat blood disorders, arthritis, breathing issues, chronic allergies, cancers, skin diseases, eye problems, and immune system illnesses.
Tooth Decay
Cough drops, chewable vitamins, and other liquid medications often contain sugar. As a result, long-term use of sweetened medications can result in tooth decay. If possible, switching to sugar-free medications can help prevent decay, especially in children. It is also essential to brush with fluoride toothpaste twice a day and floss regularly. Additionally, you should visit the dentist for professional teeth cleanings every six months.
Cancer Treatment-Related Oral Conditions
Chemotherapy (chemo) is the most widely used cancer treatment that uses chemicals to kill cancer cells. However, there are many negative side effects of chemo. For example, hair loss, weight loss, vomiting, and nausea commonly occur. Chemo can also cause a variety of oral health side effects, including:
- Dry mouth
- Changes in taste
- Cavities, which are also called “tooth decay”
- Bone disease
- Increased risk for gum disease
- Pain and inflammation inside the mouth
- Difficulties chewing, speaking, and swallowing
- Mouth sores
Turmeric for Depression & Anxiety: Is Curcumin a Good Antidepressant?
The prestigious Curcuma longa root is one of the most beneficial medicinal herbs of our time. This member of the ginger family contains turmeric, a robust rhizome with numerous healing properties.
Widely used in southern Thai and Indian cuisine, turmeric is now getting recognition as more than just a kitchen spice. But, can turmeric help depression, anxiety, and stress relief?
Turmeric for Depression and Anxiety
Turmeric’s versatility as an Ayurvedic herb has shown promise for many ailments, including arthritis, weight loss, and inflammatory skin conditions like psoriasis and eczema.
Recent studies on the benefits of turmeric allude to the possibility that it may also serve as a complementary treatment to several neurological disorders. Researchers believe curcumin can help prevent Alzheimer’s disease, reduce symptoms of epilepsy, and delay the onset of other neurodegenerative conditions.
We’ve also seen evidence suggesting that turmeric can help stabilize mood and combat depression. If you’re dealing with anxiety or severe fluctuations in perceived quality of life, curcumin might be the supplement need. (1)
Before we dive into the studies and turmeric’s mechanism of action, let’s look at anxiety and depression in a bit more detail.
What is Depression?
Depression, otherwise known as clinical depression or major depressive disorder, is a common mood disorder. Its impact on daily life can be profound. It can change how you think, how you feel, how you act, as well as your ability to sleep, eat, and work.
Symptoms can vary between individuals, but for the most part, there’s a lot of overlap among depressed individuals. Feelings of hopelessness, worthlessness, pessimism, emptiness, a sense of being alone, and even suicidal thoughts are all severe and require immediate attention.
There are a few different types of depression to keep in mind as we proceed through the article.
- Persistent Depressive Disorder: Otherwise known as “dysthymia,” is a depressed mood lasting a minimum of two years. Symptoms may be less severe at times, but the depression is persistent.
- Postpartum Depression: Women who experience major depression amidst pregnancy or following the delivery. Extreme sadness, exhaustion, and anxiety often occur.
- Psychotic Depression: Transpires during bouts of severe depression while simultaneously experiencing some form of psychosis— false fixed beliefs (delusions), hearing or seeing things (hallucinations).
- Seasonal Affective Disorder: This type of depression arises during seasonal changes, particularly during winter months, when sunlight is less frequent. It usually dissipates during summer and spring months.
You may possess a higher risk of developing the disorder if you have a family history of depression. The odds also increase if you’ve undergone significant life changes, stress, or trauma, or if you’re dealing with illnesses or medical problems.
Severe medical conditions such as cancer, heart disease, diabetes, and Parkinson’s can all worsen when they co-occur with depression. Thus, it’s critical to seek medical attention as soon as possible if you’re experiencing symptoms of depression. (2, 3)
What are Antidepressants?
Prescription antidepressants are supposed to correct the chemical imbalance in the brain responsible for depressive symptoms. Specifically, these drugs will impact the level of serotonin, the “feel-good” neurotransmitter in the brain. But there’s a catch.
Evidence suggests the majority of the positive benefits from antidepressants derive from the placebo effect. Some drugs increase the level of serotonin, while others decrease the level of serotonin. Yet, they all show similarly positive results. This fact seems to fly in the face of the chemical imbalance theory. (4)
Nevertheless, studies indicate that turmeric possesses an antidepressant effect in the brain without the plethora of side effects that accompany prescription medications. (5)
Why Turmeric Curcumin?
There is now an abundance of research suggesting that depression is an inflammatory disease that develops as a result of chronic low-grade inflammation and oxidative stress. (6, 7)
Turmeric has a well-documented status as one of the best over the counter anti-inflammatory agents. Also, curcumin’s antioxidant properties can help reduce oxidative stress, a primary cause of depressive disorders.
In this post, we’ll explore the science and research behind curcumin’s ability to stabilize our mood, reduce stress, and help major depressive disorder.
Turmeric and Depression: Can Curcumin Reduce Anxiety and Stress?
One study sought to uncover the antidepressant activity of curcumin on 60 patients with major depressive disorder (MDD). The trial split the patients into three groups where they received either fluoxetine (20 mg), curcumin (1,000 mg), or their combination for a 6-week treatment period.
Fluoxetine is a prescription antidepressant classified as a selective serotonin reuptake inhibitor (SSRI). This class of drugs seeks to raise serotonin levels in the brain to correct potential chemical imbalances in depressed or anxious individuals.
The study used the Hamilton Depression Rating Scale (HAM-D17) to assess response rates and mean change in the three groups. The results showed the following:
- 8% response in the combination group
- 7% response in the fluoxetine group
- 5% response in the curcumin group
Even though the combination of curcumin and fluoxetine scored best, the results were not statistically significant. Also, the mean change in the HAM-D17 score was comparable in all three groups. This conclusion suggests that turmeric may help treat patients with MDD, effectively, and without adverse side effects. (8)
Another human study tested 123 individuals with MDD in a double-blind, placebo-controlled, and randomized environment. Researchers split the subjects into four different groups and treated with either a placebo, 250 mg of curcumin, 500 mg of curcumin, or 250 mg of curcumin plus 15 mg of saffron.
The results showed that the three active drug treatment groups had greater antidepressant effects than the placebo. There were no significant variances in efficacy among the medicated groups. (9)
A third human trial assessed curcumin’s antidepressant activity on a group of 108 men between 31 and 59 years of age. The subjects took either 1,000 mg of curcumin or a placebo for a 6-week treatment period.
Chronic supplementation of turmeric resulted in a strong antidepressant behavioral response in the group compared to placebo. This study also used the HAM-D17 rating scale and noted significant improvements in the curcumin group. (10)
Turmeric appears to influence multiple biological mechanisms linked to major depression, such as oxidative stress pathways and immune-inflammatory activity. Curcumin also modulates monoaminergic action, which is responsible for regulating neurotransmitters, namely dopamine, serotonin, norepinephrine, and epinephrine.
Next up is a randomized and double-blind trial containing 56 individuals with major depressive disorder. The subjects treated with either a 500 mg dosage of curcumin two times per day or a placebo for eight weeks. Two scoring systems measured the efficacy of turmeric on MDD symptomology during the study.
The results showed both curcumin and the placebo group yielded improvements from baseline to week four. However, from week four to eight, curcumin was substantially more effective than placebo at enhancing anxiety and mood-related symptoms. (11)
Further research examined the behavioral effects of curcumin in animals with chronic stress. By subjecting a rat group to chronic stress protocol for 20 days, there was a notable performance dip in the shuttle-box task, accompanied by several adverse physiological effects. The unwanted behavioral and physiological changes reversed themselves with curcumin administration. (12)
A similar trial also found significant behavioral improvements in a group of mice with Post-traumatic stress disorder (PTSD) once curcumin entered the frame. After a 14-day treatment period with turmeric, the mice experienced the reversing of serotonin (5-HT) dysfunction. This result suggests the anxiolytic-like effects of turmeric may be beneficial for psychiatric disorders. (13)
Another animal study tested curcumin’s antidepressant mechanism of action on a group of mice. When administered with various antidepressant drugs, such as fluoxetine, venlafaxine, and bupropion, curcumin and piperine enhanced the anti-immobility effect. The study also noted a synergistic increase in serotonin levels. (14)
DHA is an essential consideration of brain health. Diets deficient in docosahexaenoic acid (DHA), a type of omega-3 fatty acid, have been linked to several cognitive disorders. DHA is essential for brain function, development, and neuroprotection. This fatty acid also plays a crucial role in the prevention of anxiety disorders and even depression.
Studies found that curcumin enhances DHA synthesis from its precursor, alpha-Linolenic acid (ALA). Turmeric also raises levels of enzymes involved in DHA synthesis. When supplementing curcumin and ALA together, one study demonstrated an anxiety-reducing effect in the behavior of rodents. (15)
Turmeric Dosage for Depression
What is the recommended turmeric dosage for depression? The human trials we looked at today used different dosing ranges between 250 mg and 1,000 mg of curcumin per day. These ranges have demonstrated excellent safety with no adverse side effects reported among the treatment groups.
Most turmeric supplements will contain between 1,000-1,500 mg of turmeric root powder and 150-250 mg of curcumin per serving. We recommend finding something that falls within that range. Start with one serving per day, assess the effects, and titrate upwards based on need.
Final Thoughts on Turmeric for Anxiety, Stress, and Depression
Can turmeric help anxiety, depression, and stress relief? The answer appears to be, yes. While we can’t proclaim that turmeric is a cure for depression, the human studies have indicated that curcumin is a good complementary treatment. It seems to have a positive impact on neurotransmitter balance and overall cognitive function. (16)
If you’re looking for a safe, all-natural supplement with antidepressant and anxiolytic effects, turmeric may be right for you. As always, please consult with a doctor or certified medical professional to see if curcumin can improve your mental health.
—————————————–
Crossfit Might Not Be A Sport, But You’re Going To Want In by Sally Writes
Thanks to athletes such as Elijah “EZ” Mohammad, black America has some insight into the CrossFit fitness movement, which had a slow start before it exploded in 2018. While it might not replace the excitement that emanates from a basketball court or the sheer adrenaline of a college football game, there is a place for CrossFit, and that is getting you into the best shape of your life. This is not the fitness movement that’s going to compel you to turn on the telly quite like Floyd Mayweather’s shenanigans in the boxing ring, but you are going to feel good. You’re going to feel powerful. And most of all, you’re going to see washboard abs and popping delts as you’ve never seen them before.
Choose An Expert To Get You Ripped
While you might find CrossFit gyms – or boxes – mushrooming in every second garage in the suburbs, you’re going to want to look up the credential of your fitness coach before signing up for a class. A professional will know to teach you about form instead of just pushing your body to the max, which will help you prevent common CrossFit injuries such as rotator cuff tendonitis, knee injuries and tennis elbow. Form is the building block, and will allow you to use each muscle to its full potential. Once form is in place, you’ll start seeing the results as your body discovers strength and range of motion you didn’t believe existed.
Nutrition Has Benefits Of Its Own
It’s not enough to hit the gym and work through the CrossFit circuit: you’ll also want to ensure that your nutrition is balanced to provide you with the ideal fuel for your next gym session. A nutritionist can provide you with the right meal plan to get the most out of your CrossFit regime while ensuring that it meets your individual needs too. By relying on a nutritionist to work out a plan, you’re bound to get a mixture of meals that will allow you to make up calories with superfoods and nutritionally dense dishes. This will naturally exclude ingredients and meals that could do damage over the long term, such as highly-processed foods, foods high in saturated fats and sodium, and those that are high in calories but low in nutrition.
It’s More Than Just HIIT
If you’re signing up for CrossFit just for the EZ abs, a delightful side effect might be the effect it has on your health. Research shows that those who participate in HIIT along with strength and conditioning training can expect results such as better weight management, improved cognitive abilities, blood pressure regulation, and even an improvement in type-2 diabetes. There are CrossFit programs designed for men, women, children, and even seniors.
Strength is the new buzzword, and for those looking to improve their overall fitness, it’s no longer enough to just be poster perfect. CrossFit allows participants to tick all the boxes, and when done safely, it can be done until late in life.
Low-Cost Healthcare Resources: Helping Those with Limited Finances
The cost of healthcare increases every year leaving many people struggling to pay for rising insurance premiums and medical bills. In just two years (between 2015 and 2017), the cost of healthcare rose 14 percent.
The resources below provide assistance for families on fixed budgets and seniors on Medicare looking for the healthcare they need.
Medicare Rights Center – Established in 1989, the Medicare Rights Center is a nonprofit organization dedicated to ensuring people living with disabilities and older adults have access to affordable health care.
NeedyMeds.org – This national nonprofit provides a wealth of information about drug assistance programs and affordable healthcare options.
MedicareAdvantage.com – This website offers a comprehensive overview of how and when to enroll in Medicare as well as a state-specific list of Medicare information and resources.
My Medicare Matters – Created by the National Council on Aging, My Medicare Matters teaches people about the Medicare system (when to enroll, how much you’ll pay, what to expect when coverage begins, and so on).
Find a Health Center – An online tool that allows people to find federally funded health centers in their area (data can be exported to PDF or XLSX). This interactive map is also available as an iPhone application.
FreeClinics.com – A state-by state guide to finding free clinics. Offers additional information for no-cost medical clinics, affordable clinics, low-income clinics, and clinics that offer services to those who are uninsured.
Medical Cost Advocate – A healthcare cost reductive service that helps patients renegotiate medical bills as well as check billing accuracy.
Low-Cost Dental Care (NIH) – The National Institute of Dental and Craniofacial Research provides advice on how to find low-cost dental care.
Hill-Burton Free and Reduced Cost Health Care – Information about Hill-Burton free care, which is available to people below current HHS poverty levels.
PACER Center – Specializing in treating children with disabilities, PACER Center provides this resource for parents trying to locate medical treatment and assistance.
4 Best Cell Phones for Hearing Impaired (Amplified for Seniors)
Normal cell phones can really be a nuisance for hearing impaired people. It has a limited volume, poor seal for background noise, and annoying transmissions that interferes with the hearing aid. Gladly, there are Android cell phones for hearing impaired people. It has the features that a person with hearing impairment would likely appreciate as it can greatly help their ways to communicate.
What are the features to consider on the Android Cell Phones?
When you are about to choose the right cellphone for your hearing impairment, you have to check the following feature considerations:
- Compatible with hearing aids
- Allows additional amplification
- Cell phone and earpiece design
- Text mode
- Video chat and calls if sign language is needed
- Vibration alert
- Speakerphone or hands-free function
A smartphone with a hands-free function is a catch for those who have hearing impairments. It is useful to be able to adjust the volume of your phone to make it easier to hear. However, if you still have difficulties with the volume, we recommend you to download some of the best volume booster apps for Android.
We have listed a couple of Android cell phones for impaired hearing people, and we assure you that these phones will meet the criteria. Of course, these are the best in class! Click Here To Read More
The Herbal Infusion “Plank Challenge” is gaining in popularity. Last week the store issued a challenge to the community to get 500 people to join them and “plank” for a minimum of 2 minutes. The youngest “planker” is 3-year old Olivia (see below).
Black or African American is defined by the Office of Management and Budget as “a person having origins in any of the black racial groups of Africa.”1 There were over 40 million African Americans in the United States in 2016—approximately 13% of the U.S. population.2
Although African Americans usually smoke fewer cigarettes and start smoking cigarettes at an older age, they are more likely to die from smoking-related diseases than Whites.3,4,5,6,7,8
Tobacco use is a major contributor to the three leading causes of death among African Americans—heart disease, cancer, and stroke.3,4,5
- Diabetes is the fourth leading cause of death among African Americans.4 The risk of developing diabetes is 30–40% higher for cigarette smokers than nonsmokers.10
Patterns of Tobacco Use
- African American youth and young adults have significantly lower prevalence of cigarette smoking than Hispanics and Whites.11
- Although the prevalence of cigarette smoking among African American and White adults is the same, African Americans smoke fewer cigarettes per day.3,6
- On average, African Americans initiate smoking at a later age compared to Whites.3,6
Secondhand Smoke Exposure
African American children and adults are more likely to be exposed to secondhand smoke than any other racial or ethnic group.12
- During 2011–2012, secondhand smoke exposure was found in:
- 67.9% of African American children aged 3–11 years.12
- 54.6% of African American adolescents aged 12–19 years.12
- 39.6% of African American adults aged 20 years and older.12
- African American nonsmokers generally have higher cotinine levels (an indicator of recent exposure to tobacco smoke) than nonsmokers of other races/ethnicities.12
Quitting Behavior
Most African American adult cigarette smokers want to quit smoking, and many have tried.10,13
- Among African American current daily cigarette smokers aged 18 years and older:
- 72.8% report that they want to quit compared to 67.5% of Whites, 69.6% of Asian Americans, 67.4% of Hispanics, and 55.6% of American Indians/Alaska Natives.13
- 63.4% report attempting to quit compared to 56.2% of Hispanics, 53.3% of Whites, and 69.4% of Asian Americans.13
- Despite more quit attempts, African Americans are less successful at quitting than White and Hispanic cigarette smokers, possibly because of lower utilization of cessation treatments such as counseling and medication.3,13
Click Here To Visit the Center for Disease Control Website To Learn More
Are You Ready To Quit Smoking? Click Here To Learn More From BlackNote.com
70+ Wonderful Uses of White Vinegar
A cancer diagnosis can be heartbreaking without adding financial worries to the mix. If bills pile up and wages grind to a halt, it can become impossible to manage expenses and can lead to an unbearable degree of stress. Amid crushing medical bills and smaller paychecks, you and/or a loved one may even face the harsh reality of a home loss.
These financial realities can wreak havoc on even the most savvy investor’s savings, but there are various assistance options that can help. If you’d like to stay in the comfort of your own home while undergoing cancer treatment, it can be a wise move, as cancer can be a temporary condition.
Sarah Manes, vice president of programs and community relations for the Angel Foundation, assists adults in active cancer treatment who live or receive treatment in the Twin Cities, Minnesota metro area. The Angel Foundation provides emergency financial assistance for non-medical expenses, and Manes says she sees a lot of families who are concerned about groceries, utilities, gas for vehicles and mortgage payments — the basics. “They’re worried about, ‘How am I going to get gas in my tank because I’m going to the Mayo Clinic five times a week and it’s 100 miles away?’” Manes says. “Or, ‘I’m one payment away from losing my house.’”
In one 2017 Duke University survey, more than one-third of 300 cancer patients who were interviewed reported that they spent more on their treatments than they had initially anticipated. Sixteen percent of those interviewed reported high or overwhelming financial stress. These individuals, who had health insurance, said they spent about a third of their total household income on health care-related costs, not including insurance premiums. More than 60% of this particular group claimed that private insurance was their primary source of health care.
A 2017 report from the Cancer Action Network reported that U.S. cancer patients paid nearly $4 billion out of pocket for cancer treatments. The U.S. spent a total of $87.8 billion in 2014 on cancer-related health care through employers, insurance companies and taxpayer-funded public programs like Medicare and Medicaid and through cancer patients and their families.
Assess your financial situation
If you’ve been recently diagnosed or if you’ve been dealing with a cancer diagnosis, now might be the time to take a few steps to evaluate whether some resources can help you straighten out your finances, help you avoid bad credit as well as foreclosure.
Step 1: Do an income and insurance evaluation.
Understand how you can manage your job and how your employer can help during a cancer diagnosis. According to cancerandcareers.org, it’s a great idea to do the following:
Know everything you can about your insurance policy. Understand what your insurance covers, and what it doesn’t. If you have your health insurance with your employer, don’t let your health insurance lapse, and always pay premiums on time. Know the details of your plan, including whether a provider is in-network or out-of-network. If you don’t have health insurance through your employer, ask yourself if you need Medicare, Medicaid or a private insurance company. Do your research so you understand the most minute details.
Know your rights under the Family and Medical Leave Act. The Family and Medical Leave Act (FMLA) is a federal law that guarantees certain employees up to 12 weeks of unpaid leave each year with no job loss threat. Employers are also required to maintain health benefits for FMLA-eligible workers.
Learn about your company’s disability plan. Understand both short and long-term disability policies. If there comes a time when you will not be able to work, you can apply for disability benefits.
Step 2: Know the costs of your treatment.
It’s best to ask questions about the expenses you’ll incur during your cancer treatment. The list of expenses from American Cancer Society can include:
- Provider visits
- Lab tests
- Clinic visits for treatments
- Procedures
- Imaging tests
- Radiation treatments
- Drug costs
- Hospital stays
- Surgery
- Home health care
Health insurance won’t cover everything, so ask your doctor and insurance company about cancer costs. It’s also possible to be proactive and ask about alternatives. For example, instead of an expensive chemo pill, your oncologist may be able to prescribe a generic drug that is just as effective.
Step 3: Calculate your monthly expenses.
Use a monthly expense calculator to analyze how your cancer care expenses will fit into the context of your overall budget. After you’ve completed these steps, you might find that you’re short on money and your home could be in jeopardy.
If you’re not sure where look for support, there are a number of programs that can help you find the right path. Kathy Conley, stakeholder engagement specialist for GreenPath Financial Wellness, offers support and guidance for people who seek to buy and keep their homes. “It’s a people-centered, holistic approach. We help people with financial wellness. We look at the whole picture as well. If you’ve got increased medical expenses, we put that into the context of the client’s whole financial picture,” says Conley.
Manage housing costs
Mortgage payments are likely one of your biggest living expenses and it can be an enormous challenge to keep up payments while fighting cancer. It’s important to work with your lender or servicer upon diagnosis. Learn about your options, which could include a short-term repayment plan, forbearance agreement, loan modification and more.
Conley says that once GreenPath gets in contact with a client, specialists do a snapshot of the financial challenges a client is facing, how long it’s been going on, what their current financial situation is and also take a look at their goals. Conley says one option could be to do a loan modification or re-amortization. More specifically, you could change the terms of your mortgage, which involves extending your mortgage term. An example could be turning a 30-year loan into a 40-year loan.
There are several ways you can shrink your mortgage payments:
- Recalculate your escrow payment. Have your mortgage company check how much you’re putting away for taxes each month. If your homeowner’s insurance or property taxes are lower, your escrow amount could be lowered and your overall payment can be lowered, too.
- Drop PMI. If you have private mortgage insurance (PMI), which is required when you put less than a 20 percent down payment on your home, find out from your lender how it would be possible to eliminate it.
- Appeal your home’s assessed value. Talk to your county officials and get your home’s assessed value lowered by checking that the county has all the information correct about your home, particularly if you think your taxes are too high.
- Look for a cheaper homeowners insurance policy. Your payments will be reduced if you lower your homeowner’s insurance rate.
- Refinance. Refinancing does cost more initially because of application fees, the cost of an appraisal, origination fees, document processing fee, underwriting fee, credit report charge, title research and insurance, recording fees, tax transfer fees, etc. but refinancing offers a long-term solution to more affordable payments. Try using a Mortgage Refinance Calculator to see how much you’ll save over the long term.
Seek additional mortgage help
You can also check to see if you qualify for mortgage assistance through Fannie Mae or Freddie Mac.
The Federal National Mortgage Association (FNMA), or Fannie Mae, and the Federal Home Loan Mortgage Corporation (FHLMC), or Freddie Mac, are government-sponsored enterprises which back many mortgages in the United States. If you have a loan through Fannie Mae or Freddie Mac, the Fannie Mae and Freddie Mac Flex Modification Program can reduce your mortgage payments through a few different options:
- You can add your past due amount to your unpaid loan balance and recalculate your monthly payments over the new loan term.
- Adjust your interest rate.
- Forbear some of the principal balance, which means a temporary payment suspension or loan modification.
To explore your eligibility, check out Fannie Mae’s loan lookup tool or Freddie Mac’s loan lookup tool.
The Hardest Hit Fund could also be a resource; it offers mortgage payment assistance if you’re unemployed or underemployed, advocates for principal reduction for more affordable mortgages, offers help when transitioning out of your home and into more affordable living.
Paying for home modifications
It may be necessary to make certain physical changes to your home during and after cancer treatment, including:
- Easy-to-reach safety rails
- Ramps instead of stairs
- Shower seats
- Hospital beds
- Over-bed tables
- Patient lifts and slings
- Trapeze bars
- Lift chairs
- Safety rails
- Lift chairs
- Elevated toilet seats
- Handheld showers
- Grab bars
Centers for Independent Living (CIL) are nonprofit agencies run by people with disabilities within local communities. CILs are free and they provide information, peer support, skills training and can also utilize assistive technology programs that can also evaluate changes to your home to help meet your needs. They generally do not sell products or charge a fee for their services.
Loans, home improvement grants and other assistance programs may be just the ticket to help you fund your modifications. Check out these websites for more information:
- Rebuilding Together
- U.S. Department of Agriculture single-family housing repair loans and grants (for very low-income individuals)
- U.S. Department of Health and Human Services
- Housing and Urban Development
Bill and utility assistance
Manes acknowledges the widespread help among government agencies and nonprofit organizations, and the Angel Foundation provided nearly 2,000 emergency financial assistance grants in 2018. “We refer to our services as the bridge that gets you to the next point,” Manes says. “A family will list out what they need help with, whether it’s mortgage or utilities, and that includes gas, water, electricity,” Manes says. “The check is cut directly to the bank or the landlord. We never give the cash or check directly to the patient. We want to make sure the money is going to the correct places.”
Similar to the Angel Foundation, utility companies often have funds to assist individuals and families. Homeowners, renters and subsidized housing tenants may be eligible for government programs and local programs in your area, and resources include:
If you need to downsize
If it’s necessary to downsize in order to manage your monthly payments, a short sale or deed in lieu could be an option to avoid foreclosure. In a short sale, also known as a pre-foreclosure sale, you sell your home for less than the balance remaining on your mortgage. If your mortgage company agrees to a short sale, you can sell your home and pay off all (or a portion of) your mortgage balance with the proceeds.
A deed-in-lieu occurs when you transfer the ownership of your property to the owner of your mortgage in exchange for a release from your mortgage loan and payments. There are some options to help you leave the home immediately, to stay in the home for up to three months without paying rent or lease the home (at market rates) for up to one year.
Other resources
Many financial aid programs and cancer organizations can help you determine the best course of action and some may also help with specific mortgage and utilities-related expenses. Do your research to find programs that fit the needs of your financial situation:
- Angel Foundation
- CancerCare
- Cancer Family Relief Fund
- Cancer Finances
- Cancer Financial Assistance Coalition (CFAC)
- Colorado Housing Assistance Corporation
- GreenPath Financial Wellness
- HealthWell Foundation
- Housing Solutions for the Southwest
- Leukemia and Lymphoma Society
- Neighborhood Assistance Corporation of America
- Operation Hope
- Patient Advocate Foundation
- Triage Cancer
- Unison Housing Partners
- Upper Arkansas Area Council of Governments
The bottom line
Ultimately, if you’re struggling with a cancer diagnosis, don’t feel as if you have to fend for yourself.
Manes says she sees people who have to make hard choices and sacrifices every day. “‘I’m sitting on $12,000 on medical bills. I’m going back to school. I have a car that broke down. I don’t think I can pay for a taxi,’” she says. “It doesn’t matter what type of cancer you have. People have to be able to get help and they need to get help now.”
Why African Americans Are More Likely to Have Diabetes
 Freelance Contribution by Sally Writes
Freelance Contribution by Sally Writes
The risk of developing diabetes is 77% greater among African Americans, according to information published in the journal Clinical Diabetes (2012). However, a recent study by researchers at Northwestern University (2018) has put an end to the mystery behind the phenomenon, finding that when all biological factors are taken into account, blacks and whites actually have the same risk of developing diabetes by middle age. The main factor that drives the difference in rates, is nothing other than obesity. The findings trumped two decades of research that had led scientists to believe that there was an unexplained reason for the differing rates.
Diabetes the Result of Cumulative Weight Gain
The study showed that if a black woman and white woman weighed the same in their 30s, their risk of diabetes at that time was the same. However, if a black woman gained more weight in the next decade or two, this would significantly increase her chance of developing diabetes. The researchers noted that the results were key, because the diabetes rate is significantly rising in black children/youths aged between 10 and 20. The causes of obesity are multiple, and include biological, social, economic, and behavioral factors. To tackle diabetes, obesity must be reduced as well, though this requires many changes that lie beyond the individual – i.e. food needs to be accessible, and there need to be enough opportunities for exercise. Greater awareness of the effects of obesity on Type 2 diabetes is also needed, so that parents can work on changing behaviors that can contribute to both conditions.
Embracing a Healthy Lifestyle
Studies have shown that a healthy diet is one akin to the Mediterranean diet, which comprises lean proteins, seasonal fruits and vegetables, and health Omega-3-rich fats, as well as whole grains. From their earliest years, children should become accustomed to the texture and flavor of whole foods, obtaining their sugar from healthy snacks and beverages like smoothies, made with fruits that are low on the glycemic index – including berries, melons, peaches, apples, pears, oranges, tropical fruits like pineapple, and dried cranberries and blueberries. These can be sweetened with stevia instead of sugar, to keep glucose levels low.
Good Sleep is Key
We have mentioned the importance of exercise and a sound diet to keep obesity and Type 2 diabetes at bay, but don’t forget the importance of a good night’s sleep. If possible, sleep in line with your body’s natural circadian rhythms. This involves sleeping when it is dark, at the same time every night. A published in the journal Diabetologia found that black women who work night shifts have a higher chance of developing Type 2 diabetes. This effect is even more pronounced in younger as opposed to older women. If you are male, don’t think you are out of the woods. A University of Chicago Medical Center study showed that black men and women sleep less than whites, men sleep less than women, and the poor sleep less than the wealthy.
We know that black people have a higher rate of Type 2 diabetes than white people, but there is no longer a mystery to be solved. The key is higher obesity rates, caused by multiple factors. To keep diabetes at bay, greater access to healthy food and more opportunities for safe and affordable exercise space are key. Finally, individual homes should work to battle diabetes through regular physical activity, a Mediterranean-style diet, and a good night’s sleep.
The Ultimate Guide to Hearing Health

Damage that occurs to our hearing and our auditory system can be irreversible, and once it happens, it can have devastating effects on our daily lives.
Hearing loss has been linked to declines in the quality of our relationships, depression and even other health concerns like heart disease.
Over time and as part of the aging process we naturally experience hearing loss at some level, but for the most part, this is a gradual decline that’s not very noticeable.
For some people, that decline can happen more dramatically than for others, or it can occur more quickly.
While it’s difficult to stop the effects of aging on hearing, there are certain things that we expose our ears to on a daily basis that might cause damage or could lead to more rapid declines in the functionality of our auditory system.
So, How Loud Is Dangerous?
One question a lot of people have is, “How loud is too loud?” If you work in noisy environments, love to go to concerts, or have been exposed to a loud blast, you may be at risk for noise-induced hearing loss.
The human ear is a fragile system, but there are measures that you can take to protect your hearing if you know you will be in a noisy situation.
85 dB SPL, which is about the sound level of heavy city traffic, is considered the upper limit for what is safe for your ears for an extended period of time.
Normal conversation usually falls around 60 dB SPL. Beyond 85 dB SPL, you should be careful to wear hearing protection for any amount of time.
The higher the noise level, the less time you should be near it without hearing protection.
Many people have experienced a temporary hearing loss or ringing in their ears after being exposed to loud noise.
This is called a Temporary Threshold Shift (TTS).

Image Source: wikimedia.org
Although it may seem harmless, a TTS is no joke.
Over time, this noise exposure will add up to cause permanent damage and irreversible hearing loss.
If you’re ever questioning if you should be wearing protection in a noisy environment, chances are, you should.
When it comes to your hearing, it is better to be safe than sorry.
Hearing protection has advanced so that it comes in many forms, including electronic earmuffs and earplugs made specifically for working, music listening, and recreation.

3 Reasons Why Asthma is More Critical for Black People
The following is a freelance contribution by Sally Writes
African Americans have a higher rate of being diagnosed with asthma in comparison to white people. Genetic factors, socioeconomic status and its effect on affordable and accessible health care, and air quality are all contributors to the increased incidence. Not only is asthma more prevalent in black people, there are some specific factors that make asthma a much more critical condition.
Acute Asthma Attacks
Asthma itself isn’t caused by poor air quality, but it can be worsened when exposed to allergens and irritants. When things like mold are present, asthma attacks are more severe and frequent because of increased irritation to the lungs and airway. While all asthma is a result of inflammation in the respiratory system, the inflammation present in African Americans is different and unique to them, according to a study by Dr. Sharmilee Nyenhuis. This causes a more critical condition from acute attacks, with blacks being 2-3 times more likely to be hospitalized. Eliminating mold, dander, and other irritants that can cause acute attacks is an important part of managing the condition.
Medication Response
African Americans are not only likely to experience more severe acute attacks, but they are less responsive to conventional medications used for treatment of asthma. Despite taking similar amounts of the same prescription medications, blacks still exhibited the aforementioned unique type of eosinophilic inflammation at an increased rate compared to whites. Evidence suggests that this difference in inflammation may impair the function of typical medications, which was supported by a study conducted at the Chicago school of medicine. This resistance to medication causes the condition to be more difficult to treat. Exploring other treatment options aside from corticosteroids should be a priority for those with difficult-to-treat asthma.
Healthcare Disparities
In addition to being difficult to treat due to medication resistance, treating asthma can be more difficult for those that are uninsured or underinsured. Black people are two and a half times more likely to fall below the poverty level; this contributes to a healthcare disparity among those whose employers do not offer coverage, and who cannot afford other options for healthcare. Access to regular check-ups, emergency care, and medication are all vital components in managing asthma. The Affordable Care Act does provide options for those with low-income, but still, people fall through the cracks, causing inconsistent treatment. Subsidies and patient advocacy play essential role in receiving stable care.
There is clearly an unfortunate distinction in the diagnosis and severity of asthma in African Americans. To combat the effects of the condition, it’s important to be armed with the knowledge to control the condition, as well as advocate for proper care and treatment.
Warning: Watching This 12-minute Video May Dramatically Change Your Life!
 The Quiet Epidemic: Our seniors are developing drug & alcohol addiction at an alarming rate. We provide information, resources and treatment for care providers and seniors battling addiction and related conditions. Click here and on the banner below to get help and learn more
The Quiet Epidemic: Our seniors are developing drug & alcohol addiction at an alarming rate. We provide information, resources and treatment for care providers and seniors battling addiction and related conditions. Click here and on the banner below to get help and learn more
Don Cornelius & The Black Male Suicide Stigma
Don Cornelius & The Black Male Suicide Stigma
In 2012, longtime host and producer of the iconic television show, Soul Train, died by suicide at the age of 75. Media reports have suggested that Mr. Cornelius took his own life due to severe pain as a result of chronic health illnesses.
One of the most prevalent views within the African-American community is that we do not intentionally kill ourselves. Many of us also believe that suicide is something only white people or spiritually-weak people do, that suicide is a cop-out, and that to even consider it is a “punk move”. However, these apparent suicides and clinical research clearly indicate that African-Americans do commit suicide.
The Sad (And Real) Facts On Black Suicide
According to the American Association of Suicidology, suicides were completed by African-Americans and that suicide was the third leading cause of death among African-American youth. The Centers for Disease Control reported that between 1999 and 2004, young African-American males had the highest rate of suicide. This latter finding is consistent with research that males are more likely to complete suicides whereas females are more likely to attempt suicide.
One reason for the difference is that men tend to choose more lethal means of death than women. But please do not take this to mean that African-American women do not commit suicide; the same 2005 data from the American Association of Suicidology reports of the 1,992 completed suicides among African-Americans that 371 of those deaths were by females. It is also important to note that, generally, there tends to be a underreporting of this behavior, so the numbers may be higher than those cited.
Why Are We Killing Ourselves?
So why do people commit suicide? At the heart of suicidal behavior is the strong desire to be free from suffering, whether that be emotional, mental, and/or physical pain. When we are hurting, we typically engage in behaviors to eliminate or at least lessen the pain. There are several risk factors that may suggest that a person is at a higher risk of committed suicide than others. Some of these risk factors are:
- male
- elderly
- chronic pain
- substance use and abuse
- chronic illness
- lack of social support
- poor response or an unwillingness to engage in mental health treatment
- having a friend or family member that committed suicide
- members of the Armed Forces who have had multiple deployments within a short time span
What To Do If Someone You Know Is In Trouble…
If a friend of a loved one has threatened to harm themselves, do not make the assumption that they are simply seeking attention. In many cases of suicide, the victim made it known to others that they were thinking about ending their lives.
Additional warning signs include:
- feelings of worthlessness
- no hope for the future
- giving away prized possessions
- withdrawing from others
- impulsive behaviors
- feeling trapped
- significant changes in mood
If any of these are present in you or a loved one, please contact the National Suicide Prevention Hotline at 1-800-273-TALK (8255).
The Black Suicide Stigma MUST Change
One of the main differences I have observed in people who have committed or have attempted suicide and others is access to a wide range of resources and the belief they can utilize them. In treatment by a qualified mental health professional, one learns various coping skills to address the causes of their suffering and is provided the support and guidance to put these skills into practice.
The deaths of bright celebrity starts, including Seau and Cornelius are truly heartbreaking…as are the countless deaths of others in the African American community who felt they had nowhere else to turn. Until the Black community takes bolder steps to abandon this crippling suicide stigma, many of the medical community fear that these tragic statistics will only increase.
Are You Having a Midlife Crisis? Mr. Free Spirit Explores This Topic
Mr. Free Spirit ends 2018 with a subject that will address men before and during that age of retirement. Have a HAPPY NEW YEAR!
Mr. Free Spirit has told you about the “UP” side of retirement, however some prerequisites loom in retirement, like a midlife crisis! What is midlife crisis? A midlife crisis is different things to many people! Let’s talk about a midlife crisis for men.
Here is one definition of a midlife crisis from Wikipedia:
A midlife crisis is a transition of identity and self-confidence that can occur in middle-aged individuals, typically 45–??? years old. The phenomenon is described as a psychological crisis brought about by events that highlight a person’s growing age, inevitable mortality, and possibly shortcomings of accomplishments in life. This may produce feelings of depression, remorse, and anxiety, or the desire to achieve youthfulness or make drastic changes to current lifestyle.
The term was coined by Elliott Jaques in 1965. More modern research has shown this is not a phase that most middle-aged people experience, and some have questioned the existence of this phenomenon.
When it does occur, a midlife crisis is not actually experienced during the midpoint of one’s life, which for most average human lifespans would be after the age of 50.
Crisis vs. Stressors
Academic research since the 1980s rejects the notion of midlife crisis as a phase that most adults go through. Personality type and a history of psychological crisis are believed to predispose some people to this “traditional” midlife crisis. People going through this suffer a variety of symptoms and exhibit a disparate range of behaviors.
It is important to understand the difference between a midlife crisis and a midlife stressor. Midlife is the time from years 45 to where a person is often evaluating his or her own life. However, many midlife stressors are often labeled as a midlife crisis.
Day-to-day stressors are likely to add up and be thought of as a crisis, but in reality, it is simply an “overload.”.[4] Both women and men often experience multiple stressors because of their simultaneous roles as wives/husbands, mothers/fathers, employees, daughters/sons, etc.
Many middle-aged adults experience major life events that can cause a period of psychological stress or depression, such as the death of a loved one, or a career setback. However, those events could have happened earlier or later in life, making them a “crisis,” but not necessarily a midlife one. In the same study, 15% of middle-aged adults experienced this type of midlife turmoil. Being of a lower educational status is related to feeling stressors to a greater degree than those of a higher education level during midlife.
Studies indicate that some cultures may be more sensitive to this phenomenon than others; one study found that there is little evidence that people undergo midlife crises in Japanese and Indian cultures, raising the question of whether a midlife crisis is mainly a cultural construct. The authors hypothesized that the “culture of youth” in Western societies accounts for the popularity of the midlife crisis concept there.
Researchers have found that midlife is often a time for reflection and reassessment, but this is not always accompanied by the psychological upheaval popularly associated with “midlife crisis. Those who made career or jobs changes early in life were less likely to experience a crisis in midlife.
The condition may occur from the ages of 45–? Midlife crisis last about 3–10 years in men and 2–5 years in women. A midlife crisis could be caused by aging itself, or aging in combination with changes, problems, or regrets over:
- work or career(or lack thereof)
- spousal relationships (or lack thereof)
- maturation of children (or lack of children)
- aging or death of parents
- physical changes associated with aging
Midlife crisis can affect men and women differently because their stressors differ. An American cultural stereotype of a man going through a midlife crisis may include the purchase of a luxury item such as an exotic car, or seeking intimacy with a younger woman. Some men seek younger women who are able to procreate, not necessarily with an intention to produce offspring. A man’s midlife crises is more likely to be caused by work issues, a woman’s crisis by personal evaluations of their roles. Even though there are differences between why men and women go through a midlife crisis, the emotions they both encounters can be intense.
One of the main characteristics of a midlife crisis perspective, is one assumes that their midlife is about to be eventful, usually in a negative way, and potentially stressful. Psychologist Oliver Robinson’s research characterizes each decade of life by describing frequent occurrences or situations particular to those age periods. He describes that a crisis can begin in a person’s early 20s, when they usually try to map out their whole life. Moreover, the later age period, between 50 and 60, may be a time of illness or even the thought of death. Such a deadline may convince a middle-aged person that their life needs to be lived as expected.[8]
Individuals experiencing a midlife crisis may feel:
- a deep sense of remorse for goals not accomplished
- a fear of humiliation among more successful colleagues
- longing to achieve a feeling of youthfulness
- need to spend more time alone or with certain peers
- a heightened sense of their sexuality or lack thereof
- confusion, resentment or anger due to their discontent with their marital, work, health, economic, or social status
- ambitious to right the missteps they feel they have taken early in life.
Mr. Free Spirit found out via some research technology of the 21st century has heightened midlife crisis to the point where everything is much easier with the use of the computer. However, keep in mind some men have no intentions of following through, they are just curious.
Once a man starts to satisfy his curiosity with the knowledge of his interest, he most often will never complete and/or follow through. However, a mate often becomes annoyed and seeks a permanent solution (i.e. divorce) for a temporary problem.
Empty nest syndrome may cause a man to deviate from logical thinking or wanting the children to leave home is equally as bad. Many men may want that exotic car but will only go as far as reviewing the price tag! That new-found young lady is just a dream. The grass may look greener on the other side, but the amount of water it takes to make it greener will wake up the dead. Boredom creates mental monsters, but realism sets in and the comforts of home and the bank account rains him back in.
What Causes a Midlife Crisis?
You can overcome a midlife crisis if you understand its causes. First, people may face them because of external factors.
Unresolved issues are the next trigger. People may display odd behavior because they have unmet needs. They may feel that circumstances robbed them of chances in life because his family situation deprived him of a higher education.
Debt adds to this list of push factors. Being middle-aged and having huge mortgages to pay is frightening and stressful. It may make otherwise rational people walk away from family and other responsibilities.
Also, there is grief. Coping with the death of a loved one compounds a midlife crisis. The transition can become utterly bewildering.
Finally, those with self-esteem issues may find it hard to transit from young adulthood to midlife. They probably become distant because they have feelings of inadequacy.
What are the Signs of Midlife Crisis?
Does the shoe fit?
A midlife crisis can take many forms. It can represent danger, no matter how it shows itself. You can help a loved one survive it if you recognize its signs.
- Health Scares
First, people facing midlife crises may start worrying about their health. They may run to the nearest clinic at the slightest hint of an illness.
- Tough Questions
The next sign of a midlife crisis is the raising of tough questions. Because they are at life’s crossroads, people will start asking themselves ‘Who am I?
- Comparisons
And then, they will start to compare themselves with others. Depression may set in because they may resent that they are not as successful as others or a spouse are.
- Acknowledging Time
They will have, in addition, a sense of time flying. They may suddenly feel discouraged with their lives and routines.
- Focus on Appearance
People facing midlife crises may start feeling dissatisfied with their looks because they are conscious of growing older. The obsession may drive them to try numerous weight loss programs. Also, older men and women may try to appear younger than they are. They may feel left behind, or that doing so is the only way to connect with their children. Women may start to dress younger than they are, while men may show off.
- Assigning Blame
People going through midlife crises may start to grouse over trivial matters because they feel confused about their lives. They indulge in petty grievances, like accusing spouses or friends of trying to malign or undermine them.
- Feeling Tied Down
Furthermore, people going through a midlife crisis may feel stuck in a rut, with no way to improve their situations. They believe that they have no options for a better future.
- Career Change
Moreover, those who have reached their middle years may feel that their jobs are dreary and want to change them. They may want to follow their passions and launch careers that they did not get a chance to before.
- Depression
Middle-aged persons may also experience depression because they realize that they are getting older. The thought of death may scare them.
- Having Affairs
Finally, people experiencing midlife crises may crave romantic attention. The boredom that sometimes accompanies years of marriage may overwhelm them and they may seek new partners.
Next month Mr. Free Spirit will fuse Midlife Crisis with Retirement relationships.
Mr. Free Spirit Out! (The past is not a place I want to visit!)
Keto Diet Fundamentals
You’ve heard of the keto diet. Everyone from Lebron James to the Kardashians has used the low-carbohydrate, high-fat diet for reasons like performance and weight loss.
The goal of the keto diet is to get the body producing ketones– a fundamentally different energy source than the carbohydrates and fats your cells typically use for energy. It can take several days of ketogenic eating before the body starts to produce ketones. And the time it takes to get into ketosis varies between individuals.
“Keto” comes from the word “ketogenic.” This is a nuanced term meaning that the body is producing ketones from fat.1 When blood ketone levels exceed 0.5mM, the body has achieved “ketosis.” So ketosis can be achieved either through diet or fasting (meaning the body is producing its own ketones to be ketogenic), or also by consuming products that raise blood ketone levels (like HVMN Ketone or ketone salts or MCT oils).
Limiting carb intake and protein intake encourages the body to burn fat–and thus produce ketones. Importantly, restricting proteins as well as carbohydrates limits the amount of substrate available for gluconeogenesis. This is the process of making glucose from non-glucose molecules such as lactate, glycerol, or protein.
Because the ketogenic diet is low-carbohydrate, it often gets confused with other low-carb diets out there. Just because a diet is low carb doesn’t mean it’s keto. It’s subtle differences in the macronutrients provided in the diet determine if the diet is ‘ketogenic.’
A macronutrient is something humans consume in large quantities to provide the bulk of energy to the body. The primary macronutrients are carbohydrates, fats, and proteins. For a diet to be ketogenic, it must be high in fat, low-moderate in protein, and very low in carbohydrates.

Here are some helpful definitions of diets with an element of reduced carbohydrate intake:
Ketogenic Diet
- The aim is to trigger the production of ketones in the body
- High fat, low/moderate protein, and low carbohydrate
Low-Calorie Ketogenic Diet
- The aim is to severely restrict calories to a level below the basic metabolic needs (i.e., <800 kCal)
- Even if this diet is relatively high in carbohydrates, the calorie deficit created can still lead to a state of ketosis
- Not sustainable long-term
Low-Carbohydrate Diet
- Defined in medical literature as a diet with < 30% energy from carbohydrates2
- May not lead to ketosis as the carbohydrate and protein intake could be too high
Atkins Diet
- This diet has several phases
- Initially, the aim is to restrict the carbohydrate intake to less than 20g per day. This degree of restriction is likely to lead to ketosis, although this is not an explicit aim
- Subsequently, the diet reintroduces carbohydrates to a level “the body can tolerate”3
- Less restriction on protein compared to a ‘true ketogenic diet–high fat, moderate protein, low carbohydrate.
Paleo Diet
- The aim is to limit the diet to foods that would have been available to Paleolithic man4
- Wide variability in interpretations
- Foods allowed include vegetables, fruits, nuts, roots, and meat
- Foods excluded include dairy, grains, sugar, legumes, processed oils, alcohol, and coffee
- No structured macronutrient target; however, following a Paleo diet results in higher protein and fat consumption than an average diet
Now you have a grasp of what makes the ketogenic diet unique–but where’d it start?
The History of the Ketogenic Diet
Fasting and Early Pioneers of the Ketogenic Diet
The concept of fasting (taking in zero calories) predates the ketogenic diet as we now understand it. Many of the benefits of fasting are likely due to the presence of ketones in the body.
Since the earliest days of man, fasting has been used as a tool to physically and spiritually cleansing.
The Bible describes fasting as a treatment for convulsions. The ancient Greek philosopher Hippocrates said, “To eat when you are sick is to fuel your sickness.”
Early advocates of fasting were obviously unaware of ketosis as a crucial factor in the anticonvulsant effect of fasting. In the early 1900s, physicians at the Mayo Clinic observed a link between a low-carb diet and fasting. They discovered that severely restricting dietary carbohydrates and increasing fat intake could decrease seizures in the same way as fasting.5 It was not until the mid-1900s, when scientists could measure ketones, that we understood fasting led to the presence of ketones in the body.
Epilepsy was not the only disease historically treated with a low-carbohydrate, high-fat diet. Low-carbohydrate diets were also advocated for patients with diabetes and obesity. Before the discovery of insulin in 1921, diabetes was managed through carbohydrate restriction. William Banting, an obese British mortician, popularized the weight loss benefits of a diet “stripped of starchy foods” in a pamphlet called “Letter on Corpulence, Addressed to the Public.”
The Dark Ages for the Ketogenic Diet
To many, a low-carbohydrate and high-fat diet is a counter-intuitive approach to support health. There is a widespread fear dietary fat is linked to obesity, high blood pressure, high cholesterol levels and other associated health complications.
In 1953 Ancel Keys, an American biochemist published an epidemiological study that introduced the “diet-heart” hypothesis. The study claimed dietary fat was a key risk factor in developing heart disease. The “diet-heart” hypothesis proposed blood LDL and cholesterol derived from dietary fat accelerates the development of atherosclerotic plaques.6
His work came at the time that US President Dwight Eisenhower, suffered a heart attack.
Following the advice of his physician, Eisenhower publicly cut back his fat intake. Nutrition was in the spotlight and Keys was able to further his hypothesis.
This led to radical changes in global food policy and public practice.
In 1977, the USDA Dietary Goals for Americans recommended a decrease in dietary fat intake, and a diet based on grains and cereals.7
At the time, there was still no clinical evidence supporting Keys’ “diet-heart” hypothesis. Subsequent large trials, including the Framingham Study and Women’s Health Initiative Randomized Controlled Dietary Modification Trial, failed to illustrate decreasing dietary fat lowered the risk of heart disease.8,9
Obesity rose following the adoption of the USDA guidelines. Some investigators hypothesized that increased dietary carbohydrates were responsible for the developing health crisis. John Yudkin, a British physiologist and nutritionist, described this phenomenon in his book “Pure, White and Deadly”10–the widespread fear of dietary fats caused scientists and nutritionists to overlook the role of sugar and starch.
Resurgence of ‘Low-Carbohydrate’ Diets
‘Low-fat’ dieting was widespread in the late 1900s. During this time, Dr. Robert Atkins became an infamous spokesperson for the keto diet. Dr. Atkins brought his version of the ketogenic diet to the masses in his 1972 book “Dr. Atkins’ Diet Revolution.” In his 40 years of practice, Dr. Atkins treated an estimated 60,000 patients for obesity and related conditions. At that time, there were no clinical studies to validate the benefits of the diet. Many patients reported side effects while starting the diet, including fatigue, weakness, dizziness, headache, and nausea. This uncomfortable induction phase was labeled the ‘Atkins Flu.’
After Atkins’ death in 2003, others started to promote the ketogenic diet for health. The Atkins Foundation recently funded a group of scientists to study the effects of the Atkins diet formally. This group of scientists includes Jeff Volek, Stephen Phinney, and Dr. Eric Westman. They discovered that the Atkins diet outperformed a diet based on the 1977 USDA guidelines with respect to measured coronary risk factors, including decreased low-density lipoprotein-cholesterol and total blood saturated FFA alongside increased high-density lipoprotein cholesterol.11 This outcome may be due to the decrease in carbohydrate and concomitant changes in the hormonal milieu, or due to effects of ketone bodies on substrate metabolism.
The pendulum of public perception begun to swing in favor of diets higher in fat, thanks to the emergence of influential writers and speakers such as Gary Taubes, Robert Lustig, and Nina Teicholtz, and clinicians and scientists such as Professor Tim Noakes, Dr. Jason Fung, and Professor Thomas Seyfried. The work of these individuals exposed flaws in the ‘diet-heart hypothesis.’
These influencers helped expose corruption in the political decisions that resulted in the last decades of vilification of dietary fat. Evidence illustrating the role of high dietary carbohydrate intake in the development of obesity and diabetes has started to grow. Much of the recent research suggests that low-fat diets may be harmful to health. This culminated with a recent meta-analysis of data from 18 countries, which linked increases in carbohydrate intake with increases in mortality.12
The fear of fat has continued to reverse. Over the last few years, the ketogenic diet has grown in popularity. Popular culture is starting to recognize and adopt the keto diet, and online searches have grown. More and more doctors now encourage and prescribe the ketogenic diet to treat metabolic disorders and obesity. Large online commmunities bring thousands of people together to discuss research, share keto diet before and after photos, and encourage each other.
Keto Diet for Weight Loss
The ketogenic diet can be used to help with weight loss and also to treat some diseases (discussed in detail elsewhere). Recently, the number of positive keto diet reviews has increased. The rising popularity of the diet has led to a demand for further randomized control trials to study its long-term efficacy. A key reason why the ketogenic diet helps weight loss is that it decreases hunger. This makes it easier to maintain a calorie deficit. It is important to stress that the overconsumption of calories will prevent weight loss, regardless of the macronutrient composition.
There’s a ton of misinformation out there about the keto diet. We’re on top of the scientific literature. Be the first to read our commentary on the research by subscribing.
Macronutrient Composition of a Keto Diet
Macronutrients are food groups that humans consume in large quantities. They provide the bulk of the energy to the body. The primary macronutrients are carbohydrates, fats, and proteins. The macronutrient composition of a diet can be described using the mass of each macronutrient, the ratio of macronutrients in the diet, or the percentage of each macronutrient in the diet. The variety of descriptions can make things a little confusing!
For example:
- A ketogenic diet contains about 5% of energy as carbohydrates.
- A ketogenic diet has a ratio of 2-4g of fat to every 1g of carbohydrates plus proteins.
- A classical ketogenic diet contains 20-30g of carbohydrate per day
When starting off on the ketogenic diet, these are good target macronutrient ratios:

Examples of food rich in:
- Carbohydrates: bread, pasta, potatoes, cereals, sugary food (sweets).
- Fat: oils (olive oil, coconut oil), butter, fatty cuts of meat, brazil nuts, macadamia nuts, avocado.
- Protein: beef, chicken, pork, fish, milk, cheese, yogurt, eggs.
Carbohydrates
The main function of dietary carbohydrates (‘carbs’) is to be a source of energy. Some say that dietary carbohydrates are not ‘essential’ as they can be made from dietary protein and fat.13

Carbohydrates are biological molecules that contain carbon, hydrogen, and oxygen, usually with a 2:1 ratio of hydrogen:oxygen. Carbohydrates occur as a collection of single units (monosaccharides, e.g. glucose), two molecules joined (disaccharides, e.g. sucrose), and chains of molecules (oligosaccharides and polysaccharides).
When following a ketogenic diet, the carbohydrate intake should be very low.
This contrasts with the modern western diet, where most dietary calories come from carbohydrates. Consuming carbohydrates causes insulin release, which inhibits ketone production in the liver and thus ketosis. Therefore, monitoring and modulating your carbohydrate intake is an important part of following the ketogenic diet.
Dietary carbohydrates replenish the stores in muscle and liver (glycogen). It also maintains blood glucose concentrations to provide fuel for the whole body, but most importantly for the brain.
Blood glucose is easy to measure using a handheld blood glucose monitor. Normal blood glucose levels fluctuate throughout the day and vary between individuals. Therefore, it is useful to track over the long term and in response to different ‘challenges,’ such as a meal or exercise.
Ranges of Blood Glucose levels for clinical diagnosis are as follows:14
- Fasting: healthy = 4-6 mM / 70-110 mgDl
- Fasting: diabetic = ~ 7 mM / 125 mgDl
- 90 minutes post-meal: healthy = < 8 mM / 140 mgDl
- 90 minutes post-meal: diabetics = > 11 mM/ 200 mgDl
When you’re following the ketogenic diet, key concepts are the total amount of carbohydrates, the ‘net’ amount of carbohydrates (accounting for the accompanying fiber), and the speed with which carbohydrates raise blood glucose (glycemic index).
With a standard ketogenic diet, it’s recommended to keep the total amount of carbohydrates limited to less than 5% of energy intake.15 See the table above for a calculation of the advised carbohydrate intake grams for a 2000 kCal per day 4:1 ketogenic diet.
Dietary fiber is carbohydrate-based material from plants that is not entirely broken down by the small intestine. Instead, it passes to the large intestine, and either undergoes fermentation (which supports the growth of beneficial bacteria),16 or excretion.
Fiber is a significant part of a well-formulated ketogenic diet. It helps to maintain gut health, and also increases food bulk and helps with the feeling of ‘fullness.’ Green and cruciferous vegetables are rich in fiber and are helpful to include in a ketogenic diet.
Depending on how ‘complex’ the source of fiber is, it has different assumed caloric values. One approach is to treat fiber as having the same amount of calories per gram as carbohydrates: 4 kCal/gram. However, as a proportion of fiber is not digested, other approaches use a lower value of 2 kCal/g. Digestion-resistant fiber does not contribute to calorie intake, as it is not broken down.
Net carbs refer to the mass of total carbohydrates, minus the total fiber, which could be a better metric to judge carbohydrate intake because:
- Fiber is mostly digestion-resistant and so should not increase blood glucose.16
- Studies have shown an increase in fiber does not affect blood ketone levels.17
The ‘glycemic index’ is a scale that ranges between 1 and 100, and it indicates how quickly food raises blood glucose after consumption. Pure glucose is the reference and is set at 100 (i.e. raises blood glucose quickly). Other foods have a comparatively lower value as they raise blood glucose more slowly. Example values for the glycemic index of food are white potato: ~80, white bread: ~75, apple: ~35, peanuts: ~15.
‘Glycemic load’ accounts for both the speed of carbohydrate release and the TOTAL amount of carbohydrates in food.
Glycemic load = (total carbohydrates (g) x glycemic index) / 1000.
Food can have a relatively high glycemic index (i.e. carrot = 47) but because the total carbohydrate amount is low (carrot = 5g per serving), the glycemic load of one serving is very low.
The “glycemic index” is a 1 – 100 scale indicating how quickly food raises blood glucose after consumption. Pure glucose is the reference and is set at 100 (i.e. raises blood glucose quickly). Other foods have a comparatively lower value as they raise blood glucose more slowly.
Example values for the glycemic index of food are white potato: ~80, white bread: ~75, apple: ~35, peanuts: ~15.
“Glycemic load” accounts for both the speed of carbohydrate release and the total amount of carbohydrates in food.
Glycemic load = (total carbohydrates [g] x glycemic index) / 1000.
Food can have a relatively high glycemic index (i.e. carrot = 47) but because the total carbohydrate amount is low (carrot = 5g per serving), the glycemic load of one serving is very low.
Proteins
Proteins are large molecules composed of chains of amino acids. The functions of dietary protein are:
- Building structural and functional components of cells
- Conversion to glucose via gluconeogenesis
- Top up intermediates in other metabolic pathways, such as the Krebs Cycle

While it is possible for a protein to be used as a fuel, this isn’t its primary function.
When following a ketogenic diet, there must be a balance of sufficient protein to maintain muscle mass. If dietary protein exceeds 20-25% of calories, gluconeogenesis from protein can stop the ketone production. Initially, target a protein intake of 0.8-1.2g per kilogram of body weight. This target balances the need for protein against the chance of excess gluconeogenesis.18
Some individuals (such as strength or endurance athletes) may have higher protein requirements. They might require a modified ketogenic macronutrient ratio of 2:1 fat:non-fat (where 65% of energy is fat, 30% is protein, and 5% carbohydrate) and can still be effective for therapeutic ketosis.
Fats
Fat gets a bad rap. In nutrition, fat is the dietary macronutrient made up of triglyceride molecules. The main functions of fats in the diet are to provide increased energy levels and makeup key functional and structural parts of the human system.

But we often misuse the word “fat.” There’s a difference between fat in cells and different types of fat molecules:
- Adipose tissue: the tissue that stores energy as fats/lipid droplets inside adipocytes (fat cells). This is body fat
- Adipocytes: individual cells that store fats/lipids
- Lipids: the most general term for insoluble and polar biological fat molecules. The lipid class of molecules includes mono-, di- and triglycerols, cholesterols, and phospholipids
- Triglycerides: a lipid molecule made up of glycerol (that acts as a backbone) joined to three fatty acid molecules
- Fatty acids: a molecule composed of a chain of carbon atoms bonded to one another with a carboxylic acid at one end
To be specific, our diet includes many sources of lipids.
Lipids are digested and travel in the blood as triglycerides and fatty acids before being used as a fuel, or stored by adipocytes in adipose tissue. Dietary lipids undergo many tightly regulated metabolic steps before storage in adipose tissue. Dietary fat does not equal stored body fat.
Triglycerides are the most important source of energy in a ketogenic diet. They account for > 70% of dietary calories. For those following a ketogenic diet, it’s helpful to understand how the lipid source in the diet is processed in the body.
Fatty acids can be saturated (no double bonds between carbons), or unsaturated (one or more double bonds between carbons).
Saturated fats are relatively stable and tend to be solid at room temperature (i.e. lard, butter, coconut oil). Historical guidelines recommended limited the intake of dietary saturated fats because fat consumption was thought to be associated with heart disease and high blood pressure. However, emerging research has shown saturated fat can have beneficial effects on blood biomarkers (i.e. increase ‘healthy’ HDL levels).12
Unsaturated fatty acids can be further divided into monounsaturated fats (only one double bond between carbons) and polyunsaturated fats (multiple double bonds between carbons). The number of double bonds is important as it determines how the fatty acid behaves both inside and outside of the body.
They tend to be liquid at room temperature (i.e. vegetable-based fats such as olive oil). Unsaturated fats are thought of as healthier than saturated fats (also known as “healthy fats”). Increased consumption of mono- and polyunsaturated fats have been linked to improved blood biomarkers (i.e. lower blood triglycerides).19 Eating enough unsaturated fats is important when following a ketogenic diet.
Increased fat consumption is not associated with cardiovascular disease.20
Eating a moderate amount of saturated fat is unlikely to be as harmful as previously believed, and saturated fat consumption as part of a ketogenic diet is unlikely to increase the risk of cardiovascular disease.
Trans-fats are produced artificially when hydrogen is added to unsaturated fatty acids in order to solidify it and make it last longer. Because of associations with poor health outcomes, these artificial fats had their generally regarded as safe (GRAS) status removed in 2015 by the FDA. 21 Avoid high levels of trans-fat consumption by eating a diet based around whole foods.
Essential fatty acids are important to include in the diet because the body cannot naturally produce them. This group includes poly-unsaturated omega 3, omega 6, and omega 9 fatty acids.
It’s believed the anti-inflammatory effects of essential fatty acids may have broad benefits for health and performance. Oily fish, such as sardines and mackerel, and seeds (i.e. flax) are good dietary sources of essential fatty acids.
The number of carbons in the fatty acid chain also has an important effect on its metabolism. The carbon chain of fatty acids can be up to 28 carbons atoms long. If there are > 13 carbons in the fatty acid, it is called a long-chain fatty acid, between 8-12 is a medium-chain fatty acid, and under 5 carbons is a short-chain fatty acid.
The body metabolizes fats differently according to chain length. Long-chain fatty acids are absorbed and go from the gut into the lymphatic drainage system and from there are released directly into the blood.
By comparison, medium- and short-chain fatty acids do not go into the lymphatic system. They travel in the blood from the gut directly to the liver.22 If a large amount of these short- and medium-chain fats are delivered to the liver at once, this can trigger the liver to convert them into ketones, even without dietary carbohydrate restriction.
Medium-chain fatty acids are highly ketogenic. They can be found in natural sources such as coconut oil or in an artificially purified form. However, for many people, consuming a high amount of medium-chain fatty acids can cause an upset stomach. This limits their use to raise ketones artificially.
When integrating these concepts into a ketogenic diet: target the majority of dietary calories as fat.
Aim to include a variety of fats from different animal and plant sources (i.e. red meat, poultry, fish, dairy, olive oil, coconut oil, nuts, and avocados).
Conversely, micronutrients must be obtained in the diet in small quantities, but are essential to health. Vitamins and minerals are examples of micronutrients.
Micronutrients in a Ketogenic Diet
When following a ketogenic diet, it is important to be mindful of micronutrient intake because:
- Reducing carbohydrate intake can lower consumption of micronutrient-rich foods (i.e. fruits and vegetables)
- In the initial 28 days of following a ketogenic diet, the balance of some micronutrients (such as sodium, potassium, magnesium, and calcium) can become disturbed due to an increase in their excretion.23 The body resolves this issue naturally after adapting to the diet
Sodium is the principal cation in extracellular fluid. Its functions are related to blood volume maintenance, water balance, and cell membrane potential. Sodium is also essential for acid-base balance and nerve conduction.
The level of sodium can fall at the start of a ketogenic diet. Adding extra sodium to meals (like adding salt or consuming bouillon/ bone broth) can reduce the chances of feeling the common side effects associated with low sodium (like cramps).
Potassium is the principal cation in the intracellular fluid. Its primary functions are related to maintaining cell membrane potential and electrical activity in cells such as neurons and cardiomyocytes.
As with sodium, levels of potassium fall at the initiation of a ketogenic diet due to increased excretion. When starting a ketogenic diet, include sources of potassium like nuts, dark green vegetables, and avocados.
Magnesium is an essential element in biological systems, especially for nerve, muscle, and immune function. Levels of magnesium also fall at the initiation of a ketogenic diet due to increased excretion. When starting a ketogenic diet, include sources of magnesium like oily fish, dark green vegetables, and seeds.
Calcium has a role in muscle contraction and is important for cardiovascular and bone health. Calcium deficiency is less common during a ketogenic diet, as staples of the diet such as fish, cheese, and leafy greens are rich sources of the mineral.
Now that an understanding of the biology of the ketogenic diet has been reached, we’ve arrived at the fun part: how to start the keto diet.
Keto Diet for Weight Loss
There’s a growing consensus that the keto diet can help with weight loss.
The rising popularity of the diet has led to a demand for further randomized control trials to study its long-term efficacy. The ketogenic diet helps weight loss because it decreases hunger. This makes it easier to maintain a calorie deficit. It is important to stress that the overconsumption of calories will prevent weight loss, regardless of the macronutrient composition.
How to Start a Ketogenic Diet
Don’t try to start the diet gradually. If carbohydrate intake is moderately-low, blood sugar levels may not be enough to fuel the brain, and the presence of carbohydrate in the diet might still be enough to stop the body from making ketones.
The main objectives when starting the ketogenic diet are to:
- Restrict carbohydrates to 20 digestible grams per day or less – a strict low-carb diet
- Consume plenty of fiber
- Restrict protein to moderate levels. If possible, stay at or below 0.45 grams of protein per day, per lb of body weight (1g/kg). So about 70 grams of protein per day if you weigh ~155 lbs (~70kg). If your goal is to lose weight, aim for 1 gram of protein per kg of your target weight
- Consume fat until you are satiated
Tips for Starting the Ketogenic Diet
- Make a keto diet menu. It’s a good idea to keto meal plan before starting the diet. Make a shopping trip to stock up on a range of foods that are low in carbohydrates and high in fat
- Use an app to track macronutrient intake. Apps such as MyFitnessPal are great to get an idea of the macronutrients in common foods. There is also a range of special online keto diet calculators
- Search for a few keto recipes to adapt cooking methods. Due to the high-fat consumption required to get into ketosis, it may be beneficial to change daily staples or cooking methods. Keep an eye out for coconut oil, heavy cream, and lots of cheese
- Make an approved list of keto foods and eliminate carbohydrate-rich foods. It will be easier to follow the diet by throwing out any foods to avoid. It’s recommended to check the labels for hidden added sugars
- Consider starting the ketogenic diet within a short period (16-36 hours) of fasting (consuming zero calories). Fasting depletes carbohydrate stores and can accelerate ketone production. Click here to read more about fasting protocols
- Gentle cardio exercise (~30 minutes) or some short high-intensity intervals (10-second sprints) can deplete carbohydrate stores and speed up ketone production

Cyclical Ketogenic Dieting and ‘Cheating’
At the moment, there is not a clear answer as to whether the benefits of the ketogenic diet can be achieved by cycling on and off the diet. It’s best to stick to the diet for 1-2 months minimum to see benefits. It can take several days to get into ketosis1 and 3-6 weeks to become “fat adapted.”18
Some research indicates ~40 days on the ketogenic diet interspersed with periods of healthy eating with more carbohydrates (Mediterranean diet) could maintain weight loss.24
“Cheating,” and consuming high-carbohydrate food, quickly stops ketone production by the liver. It can then take a considerable amount of time for the body to get back into ketosis. Time taken to get back into ketosis will depend on many factors. These include the amount of carbohydrates consumed, how adapted the body is to produce ketones, activity level, etc.
However, cyclical ketogenic diets are a promising area of scientific investigation. Recently, scientists studied the effect of long-term cycling of the ketogenic diet (one week on, one week off the diet) compared to a normal diet in mice. Cyclical keto dieting reduced mid-life mortality and increased healthspan.25
Optimal Range of Ketosis
As with all processes in metabolism, the state of ketosis is a spectrum. Past a threshold (which varies from person to person), even a small increase in dietary carbohydrate intake can trigger enough insulin release to take the body out of ketosis.
Guidelines for target levels for blood ketones are:
- No ketosis: under 0.5 mM BHB in blood
- Low ketosis: 0.5 – 1.5 mM BHB in blood
- Moderate ketosis: 1.5 – 3 mM BHB in blood
- High ketosis: over 3 mM BHB in blood
Pathological ketosis: over 15 mM BHB in blood
The level of ketosis required for different physiological benefits is unknown. For endurance sports, a higher level of ketosis (~4 mM) appears to be superior to lower levels.26,27 This is possible because ketones fuel athletes.
However, some other benefits of ketosis, such as reduced appetite may be seen at much lower levels (0.5 mM).28
The best way to know if you are in ketosis is to measure the levels of ketones (BHB) in your blood. You can also estimate blood levels by measuring ketones in your breath or urine.
Physiological Ketosis
The typical methods used to generate physiological levels of ketosis are fasting, the ketogenic diet, and consuming exogenous ketones like HVMN Ketone.
After an overnight fast, a low amount of ketones (0.1-0.2 mM) can often be detected in the blood. As the time spent fasting increases, blood ketone levels slowly rise until a plateau at 8-10 mM of BHB has been reached after many days. Scientist Hans Krebs described this plateau as “physiological ketosis.”29
Fasting long-term is unsustainable, so following a strict ketogenic diet can be used to maintain a low level of continuous ketosis. Research suggests blood BHB levels between 0.4-1mM can be achieved while following a ketogenic diet.18 Anecdotal evidence suggests it’s sometimes possible to reach higher levels.
Using exogenous ketones can raise blood ketones to a physiological level without the ketogenic diet or fasting. The level of ketosis reached depends on the exogenous ketone supplement used. Reported levels range from 0.6 mM with a ketone salt or a medium-chain triglyceride supplement26,30 and up to 6 mM with HVMN Ketone.27
Pathological Ketosis
Sometimes, the body starts producing ketones as a result of a disease (pathology). This can lead to dangerous levels of ketones in the body, though these high levels are very uncommon in healthy people following the ketogenic diet.
Alcoholic ketoacidosis (AKA) is a result of chronic alcohol consumption usually accompanied by malnutrition. AKA is characterized by increased ketone production (levels > 15 mM) via liver alcohol metabolism, in conjunction with a mild elevation in blood glucose levels. Symptoms include nausea and vomiting, fatigue, altered breathing, and abdominal pain.31
Diabetic ketoacidosis (DKA) occurs most frequently in patients with type 1 diabetes. DKA is the simultaneous occurrence of high blood ketones (> 20 mM), high blood glucose, and acidification of the blood.31 It develops when insulin is absent, or insulin signaling is no longer functional.
This means the physiological state of starvation is triggered, even in the presence of high blood glucose. As during starvation, lipolysis (fat release) increases. This causes the liver to produce a high amount of ketones and blood pH to fall (as ketones are an organic acid).
As glucose levels are very high, the excess is excreted in the urine. This draws water and electrolytes out of the body, causing dangerous dehydration. Symptoms of DKA include nausea, vomiting, altered breathing, abdominal pain, and unconsciousness. The rapid onset and alarming nature of DKA is a reason why ketosis has a bad stigma in the medical community.
Who Should Avoid a Ketogenic Diet?
Following a ketogenic diet may not be suggested for people with the following medical considerations:
- Pregnancy
- Kidney failure
- Impaired liver function
- Impaired fat digestion (gallbladder disease, gastric bypass, pancreatitis)
Genetic defects in metabolism (CPTI/II deficiency, beta-oxidation defects, fatty acyl dehydrogenase deficiency)
Potential Side Effects of the Ketogenic Diet
When starting a ketogenic diet there can be a period of 2-3 days where blood glucose levels are low, but ketone production has not reached a sufficient rate to provide enough fuel for the brain.
This can result in a series of symptoms, known as the keto flu, which include:
- Headache
- Muscle cramps
- Fatigue
- Nausea
- Dizziness
Exogenous ketone supplements, such as HVMN Ketone, and medium-chain triglycerides can be used to reduce symptoms of keto flu. They provide the brain with a source of energy without carbohydrate consumption. These supplements increase the levels of ketones in the blood artificially. Exogenous ketones do not increase the body’s ketone production (called endogenous ketones) and can inhibit32 the release of fatty acids from adipocytes.
It can be initially tricky to adjust food intake to ensure adequate nutrition when following a ketogenic diet. Also, some people find the diet isn’t sustainable due to individual differences in metabolic state or lifestyle. If the diet does not provide the correct balance of macro and micronutrients, some individuals develop other symptoms beyond the keto flu after the adaptation period. These include:
- Constipation
- Bad breath
- Difficulty in maintaining physical performance
- Hair loss
- Gallstones
- Elevated blood triglycerides or cholesterol
To treat these symptoms, ensure the diet provides enough calories and micronutrients. Many people reduce fruit and vegetable consumption on a ketogenic diet (due to carbohydrate content). This means it is easy to become deficient in vitamins and to under-consume fiber.
The ketogenic diet can alter the way that the kidneys excrete electrolytes (such as sodium), so electrolyte supplementation can reduce the side effects of an electrolyte imbalance.
Possible Clinical Applications of the Ketogenic Diet and Ketosis
Some of the earliest reports of the ketogenic diet describe its use in a clinical setting.
In the early 20th century, ketogenic diets helped treat drug-resistant epilepsy. Doctors also prescribed ketogenic diets to treat type 1 diabetes before the invention of insulin.
As analytical techniques progressed, scientists learned that ketones themselves might be a crucial part of the success of the ketogenic diet to treat disease. From this finding stemmed a field of research to examine the potential benefits of ketosis in a range of disease states:
- Weight loss
- Diabetes and metabolic syndrome
- Neurological disease: epilepsy, Alzheimer’s disease, Parkinson’s disease, migraine, concussive disease, and traumatic brain injury
- Cancer
- Inflammatory diseases
While the ketogenic diet is not yet a first-line treatment recommended by doctors for any of these diseases, it’s a relatively easy and tolerable step that patients with these conditions can take to improve their health. Emerging research suggests there may be beneficial effects of ketosis for some people, and further studies are required to confirm how best to use the diet in these clinical settings.
You’re not alone. Many think they’re in ketosis but aren’t–the newness of the diet leads to misinformation online. HVMN provides the latest science around meal-timing, supplements and macronutrient composition. Subscribe and be first to know the newest techniques for keto diet results.
Scientific Citations
African-Americans Are Twice As Likely To Have Alzheimer’s or Dementia Than Whites
Warning Signs Help Ensure Early Detection and Care Planning
According to the Alzheimer’s Association 2015 Facts and Figures report, African-Americans are two times more likely to develop late-onset Alzheimer’s disease than whites and less likely to have a diagnosis of their condition, resulting in less time for treatment and planning. The Alzheimer’s Association is committed to raising awareness of Alzheimer’s disease, the nation’s 6th-leading cause of death, in diverse populations.
Alzheimer’s Association 10 Warning Signs of Alzheimer’s
- Memory loss that disrupts daily life.
- Challenges in planning or solving problems.
- Difficulty completing familiar tasks at home, at work or at leisure.
- Confusion with time or place.
- Trouble understanding visual images and spatial relationships.
- New problems with words in speaking or writing.
- Misplacing things and losing the ability to retrace steps.
- Decreased or poor judgment.
- Withdrawal from work or social activities.
- Changes in mood and personality.
About the Alzheimer’s Association®
The Alzheimer’s Association is the world’s leading voluntary health organization in Alzheimer’s care, support and research. It is the largest nonprofit funder of Alzheimer’s research. The Association’s mission is to eliminate Alzheimer’s disease through the advancement of research; to provide and enhance care and support for all affected; and to reduce the risk of dementia through the promotion of brain health. Its vision is a world without Alzheimer’s. Visit alz.org.
A Seniors Guide To Eating Health by Brenda Snow
By Brenda Snow
Healthy eating and understanding nutritional requirements are important at any age, but it can be especially important for seniors. Seniors have unique nutritional needs, but also specific dietary considerations that need to be accounted for when it comes to the foods they’re eating. As people age, their metabolism slows down, which means that for most older people they need fewer calories than they did when they were younger. It’s not just changes in metabolism that are important to understand when it comes the healthy eating for seniors, however.
As we age, our bodies change and considerations to keep in mind with senior nutritional needs can include the gastrointestinal system and dental conditions. There are also certain lifestyle elements for seniors that may play a role in their diet and nutrition.
If seniors aren’t eating a healthy, balanced diet, it can wreak havoc on their immune system, making them more susceptible to common illnesses like the flu, as well as more serious conditions. It can also lead to weight gain or weight loss, and seniors who aren’t eating a healthy diet may have reduced cognitive function and lower energy levels. It’s not uncommon for older people to experience malnutrition, in varying degrees, often because of eating too little, deficiencies in certain nutrients, or an imbalance in the diet. Even a mild level of malnutrition can lead to fatigue, lethargy, and a lack of interest in other areas of health and wellness.
For seniors who make healthy eating an essential part of their life, they’re more likely to enjoy a stronger immune system, better overall health, and a stronger quality of life.
To help seniors, their families and their caregivers ensure they’re making the right nutritional choices, I put together this guide. My goal with this guide is to help seniors live a fulfilling life, starting with a foundation of good nutrition. From the limitations that can cause seniors to have poor nutrition, to easy tips to incorporate healthy foods into your lifestyle or the lifestyle of your loved one, this guide has a lot of information that I hope will be valuable to you.
Publisher’s Note: When Mr. Free Spirit told me that he was conducting research for an article that he was writing detailing the high suicide rate for retired men, I immediately thought about the number of retired NFL football players who have committed suicide and the celebrity deaths “Soul Train” icon Don Cornelius, actor Robin Williams and former CNN correspondent Anthony Bourdain. I think that mental health awareness and education is a very important topic and something that we want to highlight here on this website.
The National Institute of Mental Health finds that men are less likely to seek support as they struggle with depression. Depression can take away anyone’s moments of peace and restfulness, but men may be statistically more likely to experience disruptions to their sleep cycles. Sleep deprivation comes with a host of other difficulties: irritability, loss of motivation, physical fatigue, compensating by oversleeping, etc. Most dishearteningly, men are more likely to be successful in taking their own lives. I want to thank Mr. Free Spirit for writing this article and I encourage everyone to be patient, caring and kind when you encounter those who struggle with some aspects of life in hopes that we can prevent them from committing suicide. For more help and information call 1-800-273-8255 or 1-800-SUICIDE.
Gary Johnson – Founder & Publisher, Black Men In America.com
Why Is The Suicide Rate So High For Men In Their Golden Years?
By Mr. Free Spirit
Since my retirement I decided to rewire and not retire. Retirement means different things to different people. Is money an important factor? YES, however other things are equally important. Nothing to do will either kill you or place you in a state of depression. Mental illness can be accelerated based on having “nothing to do.”
Did you know the suicide rate in elderly men is high?
For most people, psychological well-being increases later in life, following a well-known U-shaped curve: people report less satisfaction in midlife and more at either end of the age spectrum. Paradoxically, though, suicide rates also rise sharply. Older white men are particularly at risk.
Among Americans of all ages, 12.4 per 100,000 take their own lives each year, according to 2010 statistics from the Centers for Disease Control and Prevention. But among those over 65, the official number is 14.9, and suicide may be under-reported. Because of the stigma, “coroners will go to great lengths to call it something else,” said Patrick Arbore, founder and director of the Center for Elderly Suicide Prevention in San Francisco. “If it’s an overdose, they can call it an accident.”
Though suicides among older people have declined in recent decades, most likely because of improved screening and treatment for depression, they remain disturbingly high among men. Suicides by women decline after age 60, but the rate among men keeps climbing. Elderly white men have the highest rate: 29 per 100,000 overalls, and more than 47 per 100,000 among those over age 85.
- Males accounted for 81.5% of suicides completed by elderly African Americans (ages 65+). This percentage is mirrored by the suicides completed by elderly Caucasian men.
Why are suicide rates so high among seniors? We know that while older people make fewer suicide attempts than the young, they are far more likely to die from them, in part because they rely primarily on guns. “Younger people have more physical resilience and use less lethal means,” said Dr. Yeates Conwell, a psychiatrist at the University of Rochester Medical Center who has studied late-life suicide.
Moreover, depression is behind many suicide attempts, and “a lot of older people have problems asking for help.”
Depression can involve different symptoms in older patients, and “men are good at masking it, because we’ve been conditioned to believe it’s not O.K. to express emotional pain.”
Beyond mental illness, researchers have identified a cluster of other risk factors in late-life suicide, including physical illness and pain, the inability to function in daily life, fear of becoming a burden and social disconnection. “Things that remove older people from their social groups — bereavement, retirement, isolation — leave them vulnerable,” Dr. Conwell said.
Knowing that some readers here have announced that they want to end their lives if (or before) they are suffering, seeing that as an exercise of personal autonomy rather than mental illness, I asked both experts if they thought suicide could ever be a rational act. If life loses pleasure and meaning, with or without a terminal disease, can suicide be a legitimate response?
Both said, cautiously, that in certain situations, after a great deal of discussion and consideration, it could be — but that’s rarely what occurs.
“The proportion of older people who take their lives without a diagnosable mental illness is very, very small,” Dr. Conwell said. Because elderly suicide is generally a result of multiple factors — physical illness and depression and a recent loss, say — “if you change one of those parameters, it may tip the balance in favor of finding solutions that help you want to live.”
At the Center for Elderly Suicide Prevention, staff and volunteers handle 3,000 calls a month to the “friendship line” (a name deemed more acceptable to seniors than “suicide hotline”). They also place 3,500 outgoing calls to people considered isolated or otherwise at risk.
“We believe connections are what bind us to life, just having the opportunity to talk might shift their view of the end, temporarily. It might not have to happen today.”
Such opportunities to talk, in ways tailored to older adults, should be more widely available than they are. (One resource is the Veterans Affairs Department’s Veterans Crisis Line.) Instead, the task of trying to recognize elderly depression and encourage treatment falls largely to primary care physicians and, of course, to family members, who should always take suicidal talk seriously. When a depressed and hopeless relative commits suicide, the family must cope not only with grief but often with guilt and unanswered questions.
Now that you have read the above, you understand being rewired not retired. During your years before retirement you had a talent for some sort that you enjoyed. No matter what it was you enjoyed it. Well, now that you are thinking about retiring or you have retired. Try doing want you always wanted to do. Maybe it’s fishing, so buy some new rods and develop your skills and fish. Maybe you are good with your hands, be the local handyman. No matter what it is, don’t sit and watch grass grow or paint dry, do something!!!
Mr. Free Spirit out!!!
Humility is not thinking less of yourself, it’s thinking of yourself less.

Help, Hope, and Recovery for Addiction and Mental Illness
The Importance of Early Detection of Prostate Cancer by Sally Writes
The Importance of Early Detection of Prostate Cancer by Sally Writes
According to the Prostate Cancer Foundation, African American men are the group (out of all the men in the world) who are hardest hit by prostate cancer. Statistically, we are 1.6 times more likely to develop this disease, and over twice as likely to die from it. Because we are in a high risk group, screening for prostate cancer should start earlier, to facilitate early treatment if required. When it comes to prevention, a healthy diet and exercise can make a positive difference.
The American Cancer Society recommends that men discuss screening with their doctors at age 50 (if they are at an average risk and are expected to live at least 10 years more); at age 45 (if they are at a high risk of developing this cancer – this includes African American men and those with a first degree relative diagnosed with prostate cancer when this relative was younger than 65) and at age 40 (for men with at a higher risk because they have more than one first degree relative who had prostate cancer before the age of 65).
What Does Screening for Prostate Cancer Involve?
Normally, testing is carried out via the PSA blood test (to check levels of prostate-specific antigen) and, possibly, the digital rectal exam. If results are normal, your doctor will normally recommend that you return every year or two, depending on your PSA levels.
An Important Proviso
It is important to speak to your doctor about the pros and cons of screening; the latter can sometimes give ‘false positives’, and studies are still being carried out on the effect of screening on lowering death rates from prostate cancer.
Can Prostate Cancer be Prevented?
Although there is no sure-fire way to stave off prostate cancer, a healthy diet and physical activity can help, because research has shown that men who are overweight have a slightly lower overall risk of prostate cancer, but a higher risk of prostate cancers that are likely to be fatal. Other research has shown that a poor diet is associated with various types of cancer, and that specific foods are cancer preventive (including fruits and vegetables; bread, rice, potatoes and pasta; lean protein sources, beans and nuts; and dairy products).
Recently, researchers found that the consumption of specific foods (tomatoes, cauliflower and broccoli, soy, beans, legumes) and fish, are linked to a lower rate of prostate cancer in particular. Apple pees, red grapes and turmeric have also been found to have a preventive ability.
The Importance of Exercise
Exercise doesn’t just boost our mental health; it also helps us maintain a healthy weight, which is important when it comes to cancer prevention as a whole. Aim for between 30 minutes and 45 minutes of physical activity a day and if you have a job that involves sitting down for various hours, get up every hour and walk about, do some stretching, or run up and down a flight of steps, to boost your cardiovascular health as well.
It is vital for African American men to know that they face a higher prostate cancer risk, so they should discuss screening with their doctor. Much can be done on a lifestyle level as well, to reduce the risk of this disease, including making important dietary changes and staying physically active.
Reduce Blood Pressure Naturally by Dr. Brenda T. Bradley
Approximately, 75 million Americans have been diagnosed with high blood pressure. According to the Centers for Disease Control and Prevention, this equates to 1 in every 3 adults. High blood pressure, also known as hypertension, is a risk factor for serious health related problems. Unfortunately, many people are unaware they may have it because it usually comes with limited symptoms. Sadly, uncontrolled high blood pressure can contribute to other causes of death in the U.S., including heart attack, stroke, diabetes, and cancer.
Given this information, blood pressure should be checked or assessed on a regular basis. Two measurements are used to check blood pressure: (1) systolic blood pressure (SBP), pressure in the arteries with every heartbeat; and (2) diastolic blood pressure (DBP), pressure in the arteries between heartbeats.
| Classification | SBP | DBP |
| Normal | <120 | and <80 |
| Prehypertension | 120-139 | or 80-89 |
| Stage 1 Hypertension | 140-159 | or 90-99 |
| Stage 2 Hypertension | >160 | or >100 |
Taking medication to reduce blood pressure levels may seem like the easy way out, but it’s not the healthiest, nor is it your only option. I was diagnosed with high blood pressure several years ago and after adopting a plant-based diets, I was taken off the medication and I no longer suffer with high blood pressure and that was six years ago.
An analysis published in JAMA Internal Medicine reported that consumption of vegetarian diets was associated with significantly lower systolic and diastolic blood pressure compared to omnivorous diets. Plant-based diets are low in sodium and characterized by high intakes of fruits and vegetables, which are rich in fiber and potassium. These factors, combined with maintaining healthy weight and regular exercise, may explain lowering effects of blood pressure.
Try following a plant-based diet for at least a month to find out how well the following foods will work for you. Then have your doctor check your blood pressure:
- Whole grains – brown rice, millet, quinoa, groats, buckwheat
- Beans/Legumes – dried (if canned, avoid added sodium) black-eyed peas, kidney beans, pinto beans, lentils, chickpea, tempeh and tofu
- Vegetable – fresh or frozen varieties, broccoli, collard greens, kale, spinach, carrots, potatoes, squash, tomatoes, beets
- Fruits – fresh or frozen varieties, such as bananas, organs, apples, pear, grapefruit, strawberries, blueberries, guava, strawberries.
Overweight and obesity increase the chance of developing high blood pressure. Following a plant-based diet can assist individuals in losing weight. Avoiding animal products, and fried and high-fat foods while increasing intake of vegetables, fruits, whole grains and legumes can promote a healthy weight and improve blood pressure. Also, physical activity can help lower blood pressure. Try a brisk walk for 30 minutes to an hour at least 3 times per week. Because exercise may put added strain on your heart, always consult with your doctor before starting a new exercise program.
I welcome questions and comments.
Here’s to good health,
Dr. Bradley
References:
- Nwankwo T, Yoon SS, Burt V. Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011-2012. Centers for Disease Control and Prevention: National Center for Health Statistics. http://www.cdc.gov/nchs/data/databriefs/db133.pdf. Accessed September 6, 2017.
- Kung HC, Xu J. Hypertension-related mortality in the United States, 2000-2013. NCHS data brief, no 193. Centers for Disease Control and Prevention: National Center for Health Statistics. http://www.cdc.gov/nchs/data/databriefs/db193.pdf. Assessed September 6, 2017
Brenda T. Bradley, PhD
Certified Integrative Nutrition Health Coach
Brenda T. Bradley, PhD is an engaging and compassionate certified health coach. Through her work and passion for healthy eating and living, she decided to answer the call to become a certified health coach. Determined to break free from the Standard American Diet (SAD) which is known to do more harm than good, she set out on her journey to research food, diseases, and fitness. Her drive and determination led her to become more involved in health and fitness.
After struggling with her own health goals and learning about the body and what it needs to perform optimally, she made the switch to a plant-based diet. This diet she credits for helping her not only to lose weight, but has improved her overall quality of life. Last year she developed a new program, The 21-Day Vegan Challenge, and has recommended that clients and those struggling with weight or health issues give it a try. The 21-Day Challenge is a vegan-only food challenge that stresses the healing power of food and how its proper use can restore the body to a natural healthy state. Dr. Bradley’s goal is to inspire others to lead the charge for healthy eating and exercise.
Contact Information
Phone: (757) 784-0832
Email: Brenda@drbtbradley
Website: www.drbtbradley.com
Everything You Need To Know About Salt, Your Health, and Your Diet
By Sally Writes
Do you think you know how much salt your body needs? Salt is an element of good nutrition that seems to be talked about an awful lot. We see “low sodium” soups and “salt-free” nuts on the shelf. Piling those items into your grocery cart might make you feel that you have your salt intake under control. But did you know that milk has salt in it? How about beer? Surprising, right? Let’s get clear on just how much salt we need, what to do to keep track, and how to cut back if needed.
How Much Salt Do I Need?
The American Heart Association teaches that the most adults should ideally take is 1,500 mg of salt per day. This is equivalent to ⅔ of a teaspoon of table salt, but don’t let that fool you. Just because you aren’t sprinkling salt onto every meal, doesn’t mean that you are under the limit.
Most foods that we eat, especially prepared foods, have salt already added in. For example, one serving size of your a typical jarred tomato sauce delivers almost 500 mg of salt. That would be a third of your salt intake, just in your sauce! Add some meat, salad dressing, and a beverage to your meal, and you will find that you can quickly rack up 1,500 mg of salt intake in one meal.
The maximum amount of salt that the American Heart Association recommends is 2,300 mg. However, 70% of Americans are at risk for diseases that are linked to sodium intake, so experts say that it is better to aim for lower numbers and be safe.
However, salt is essential for our body’s functioning, so you can’t cut it out completely. For instance, it is very helpful as a home remedy to cure sore throats – by mixing with garlic and gargling, this is a great natural solution! Also, endurance athletes who lose salt through sweat will need to think about replacing their losses.
How To Track Salt Intake And Cut Back At The Same Time
You don’t need to become obsessive about adding up your salt intake all day, every day, to be healthy with regards to sodium. Instead, think about adding in more home cooking to your diet.
Consuming overly processed foods, and eating on the go can make it nearly impossible to keep track of salt intake. Often these kinds of foods are high in sodium, just to help them stay preserved. Feel in control as you see every ingredient that you put into your meals, and you’ll move to a whole new level of your health and wellness.
Instead of thinking that you are doing the right thing by purchasing “low sodium” options at the grocery store, start to learn the facts. The accurate numbers about how much sodium your body needs are surprising. Get in control of your intake by cooking meals from scratch.
The Hon. Dr. Shakiera Marilyn Hockaday-Bey
To learn more visit the Herbal Infusion website. We will have more from Dr. Hockaday-Bey over the next several weeks. Here are some of the services provided by Dr. Hockaday-Bey and Herbal Infusion.
Dr. Hockaday-Bey and Gary Johnson at the Herbal Infusion Health and Wellness Store in Ft. Washington, MD
- Improved mental clarity.
- Relief from vertigo.
- In some cases, restoration of smell and taste.
- Increased nail and hair growth. Regulation of ear pressure.
- Better lymphatic circulation.* Proper balancing of ear fluids.
- Catarrh, resulting from nasopharynx problems. Balancing of fluids that provoke headaches. Hygienic treatment of ear.
- Activates proper ear fluid circulation. Can eliminate ringing in ears. (Tinnitus) *Bouncing on a trampoline can also move the Lymph fluid….try it!
To learn more visit the Herbal Infusion website. We will have more from Dr. Hockaday-Bey over the next several weeks.
Health Benefits of Apple Cider Vinegar
By Gary A. Johnson (Posted 6-12-17)
By Gary A. Johnson (Posted 6-12-17)
I’ve been using apple cider vinegar with the “mother” for over several years and I love it. I am overweight and take medication for high blood pressure and high cholesterol. Over the years I started an exercise regimen comprised mostly of walking and cycling all year round and I take apple cider vinegar every morning. My doctor cut all of my medication doses in half and is working with me get off of all the medications within a year.
One of the best sources on the Internet with information on apple cider vinegar is Helen Sanders, the main editor at Health Ambition.com. If you want to learn more about the enormous health benefits of apple cider vinegar click on the picture below.
Here’s to your good health. Gary Johnson, Publisher – Black Men In America.com
Why Substance Abuse Among Seniors Can Be Devastating (Posted 03-09-17)
Presently, substance abuse among seniors can fall into two large groups. Firstly, the “hardy survivor”, or people who have been abusing substances for many year. Second, the “late onset”, or people who became substance abusers later in life. Regrettably, it most commonly occurs due to misuse of drugs prescribed for chronic health problems.
First and foremost, the reasons why the elderly turn to substance abuse varies. For example, They call one of the most common reasons, “the empty nest“ syndrome. The “empty nest“ refers to the void children leave once they are grown up and have moved out of their parents’ home. As a result, their absence causes a mix of new emotions. Moreover, they try to cope by implementing drugs into their daily life.
In addition, another important issue that surfaces is the issue of age. The fact that none of us is getting any younger scares them. You are no longer in your thirties, the forties, and are coming to realize fifty is a different season. Consequently, it requires a new game plan and a new set of rules. Coping with, and eventually accepting the new reality is a tough pill to swallow. One’s body is changing, and illness and pain become more common between the ages of 55 and 65.
Other reasons why elderly people choose addiction:
- Loss of a partner
- Friends are growing apart
- Immobility
- Stress
- Retirement
- Loss of financial security
- Life in a nursing home
In any case, the most common vehicle of substance abuse among seniors are alcohol and prescribed medications. In fact, people over the age of 65 use almost 30% of all prescribed drugs in the US. For example, the most common prescription drugs they abuse are sedatives, hypnotics, dietary supplements, and benzodiazepines. Seniors who use those drugs and mix them with alcohol are more likely to visit the hospital due to substance interaction. Another important issue is that they tend to share their medications with friends.
In the same way, alcohol are also a commonly abused substance amongst the elderly. It’s important to note that alcohol can interact with many prescribed drugs and cause serious adverse effects. Furthermore, seniors are more sensitive to the effects of alcohol. Therefore, they show lower tolerance to this substance. Also, older men are more likely to develop alcohol addiction than women.
Paradoxically, substance abuse of illicit drugs such as heroin among seniors is very rare. It is usually limited to people who have had addiction issues in their youth.
No doubt, along with common dangers of substance abuse, seniors are more vulnerable to the side effects of drugs. Of course, as one ages, the body cannot absorb and metabolize certain drugs so well. Consequently, as these changes occur, it becomes more difficult for one’s body to process medications. Additionally, drug interaction can make it worse and cause serious health issues. Furthermore, alcohol or drug-related injuries are more common amongst seniors. However, more often than not they refuse to ask for help due to shame or pride.
Some of the most common substance abuse signs amongst seniors are:
- Loss of appetite
- Sleeping pattern problems
- Disheveled appearance
- Weight loss
- Memory issues
- Increase of appetite
- Depression
- Sadness
- Injuries and bruises
- Lack of hygiene
- Distancing from friends and family
- Chronic pain
- Lack of motivation for everyday activities
The first challenge in rehab is to recognize the problem, and not mistake it as dementia or depression.
Usually, the best treatment solutions along with inpatient or outpatient rehab facilities are support groups and counseling. That way, the patient can get peer support and professional help. It is important that when you talk with a senior patient, you should be comforting. Additionally, you should use easy to understand language.
In conclusion, in some cases, substance abuse in the elderly is overlooked and neglected due to their age. Regrettably, ageism is a serious issue that should be remedied. Ultimately, people of all ages, backgrounds, and ethnicity deserve equal treatment.
Are you looking for good addiction treatment centers for the elderly? Follow this link to learn more about what they have to offer.
For more information visit Addiction Resource.com.
Resources for Alzheimer’s Disease
Parent’s Guide: Helping Children & Teens Understand Alzheimer’s
Preparing Your Home for a Loved One with Alzheimer’s: A Caregiver’s Guide
Another World: People With Alzheimer’s Share Their Perspectives
Alzheimer’s Aggression: Causes & Management
Guide to Addiction Prevention for Seniors
Caring for the Alzheimer’s Caregiver
Helping Alzheimer’s Sufferers Cope with the Loss of a Loved One: A Guide for Caregivers
——————————————————————–
NAKED AND NOT ASHAMED: LIVING WITH DEPRESSION
By Dr. Salim Bilal-Edwards
I was diagnosed with major depression three years ago. We all experience depression at some point in our lives, for most it is situational due to specific events such as the loss of a job, death of a loved one, or other disappointments. However, for persons with major depression it lingers and is often recurrent. Persons with major depression or what is commonly called clinical depression may have good days and not so good days. A person with clinical/major depression may go a period of time having days, weeks, or even months of good days, but then out of nowhere they fall into a funk without explanation. Often we try to mask our pain and hide in the crowd laughing and joking, and then go home to a dark house which is empty of life. Those of us with major depression are sensitive to others who we see hurting or going through a rough or difficult time. I found myself trying to help people I loved, but was not helping myself and inside my brain and emotions I was going through pure hell. A revelation came to me one day as I was suffering and trying to help a loved one. The revelation was the voice of the flight attendant giving instructions prior to take off. I was reminded of one of the major instructions which is “if the cabin loses pressure, an oxygen mask will drop from the area above your seat, put the mask on yourself first before helping the persons around you”. Those may not be the exact words, but you get the picture. I was going through my personal hell called depression trying to help others but neglecting my mental health.
THE EVILNESS OF DEPRESSION
Depression not only affects the person who is suffering, but often impacts those around them. The impact of depression on marriages and families can be devastating. As for me, not seeking help in a timely manner came at a great cost. I languished in mental and emotional agony. I am in private practice as a clinician and relationship/life coach. I would go to work and be on top of my game helping others through their rough patches, but at the end of the day I would go home and suffer in silence. I would attend church Sunday after Sunday being inspired by the Word of God, but that was short-lived as I would fall back into a funk within a day or two. I found myself easily agitated and angry at any and every one. There seemed to be two different people who were diabolically opposed to one another. I was this spiritual God-fearing man who was full of life, sought peace, and had a servant’s heart; then when depression would come upon me I was this angry agitated person who did not want to be bothered with anyone and would stay in the house alone for days at a time. However, my job demanded that I pour into the lives of clients who were coming into my office to seek help with their pain. I had to push myself to provide the best counseling and coaching possible because my oath stated that first and foremost to do no harm. I am a man of integrity, so I put on my game face, went into my office and gave the best counseling and coaching possible. I am quite good at what I do and my clients and other therapist often refer clients to me. I became good at masking my pain, but it was just that a mask.
ON AN ISLAND FEELING ALL ALONE
The hardest part of my depression was wanting help and support from my friends and family and them not being able to provide that support. You see, I had always been the strong one. I had always been the persons who everyone could depend on. So, when I was struggling with depression they didn’t know how to help. They continued to rely on me to help with their issues even though I was suffering with depression they still relied on me for help because that is what I always did “help”. I take full responsibility for allowing family and friends to pull on me because I continued the masquerade as if I was alright when I wasn’t alright. My depression was getting the best of me and I began to cancel sessions with my clients because there were days in which it was difficult to get out of bed. There were days that I was so drained that my entire body ached. After hitting a low point and having more bad days than good days, I reconciled that I needed to seek counseling again. Let’s be clear that every doctor needs a personal doctor, every lawyer needs a personal lawyer, every minister needs to be ministered to, and every clinician and life coach needs a personal clinician and life coach. As the ole saying goes “a person who have himself for a doctor has a fool for a doctor”. I was being a fool for quite some time helping people, but not getting the help I needed.
FIGHTING THE STIGMA
As a clinician, I know full well the stigma in the African American Community attached to counseling which prevents persons from seeking help. While I was not caught up in the stigma, I was acting like Superman and thought I could handle anything. The stigma attached to counseling coupled with the Superman mentality keeps most African American men from seeking counseling. As African American men, some the misconceptions of manhood are major barriers to seeking help. Growing up I can remember hearing that men are not supposed to cry and crying is a form of weakness, men are not supposed to show emotions, men should always be strong and be tough. As a young boy growing up in the inner-city of Washington, D.C. showing any signs of weakness or frailty would subject you to being picked on, bullied, and having your manhood challenged. I believe as young boys grow into adults they carry those misconceptions of manhood which become barriers to seeking counseling.
Major Depression effects more people than we realize and far too many people are unwilling to seek help. Getting help for your depression can prevent you from self-medicating. Yes, self-medicating. Too many people who are suffering with depression, instead of seeking help, turn to substance use, gambling, sex, and other deviant behaviors to mask their pain. For me, I turned to prayer and my spirituality to deal with my depression. I prayed. I attended church and bible study. I studied my Word. I prayed for others and yet God seemed silent. What compounded my depression was that I thought I was doing everything I was supposed to do by having integrity, by being faithful and obedient, by treating others nice even those who were not being nice to me, but I continued to live in this hell called depression. Yes, God is a Healer. Yes, God is a Deliverer. Yes, God is a Counselor. Yes, God is a Provider. However, God created doctors and therapist to be Angels here on earth to help us through our difficult times of depression. I was self-medicating in religion and neglected my mental health by not seeking help.
DON’T PUSH ME CAUSE I’M CLOSE TO THE EDGE:
Many people are pushed deeper into depression by the ones who supposed to love them most. The things that family and friends can say to a person dealing with depression can push a person close to and sadly over the edge. The things that are said such as “just get over it” can be debilitating to a person with depression. If the person dealing with depression could “just get over it” he or she would get over it in a blink of an eye, but it is just not that simple. Some people may have an episode of depression, that only last a few days and then back to some normalcy, whatever normal is, and some episodes of depression can last for weeks or months at a time. Telling the person dealing with depression to “just get over it” does more harm than good. Some of the labels given to persons dealing with depression can also be debilitating. Labeling a person or critiquing their behavior as lazy, attention seeking or simply manipulative is extremely harmful. Imagine Hearing your loved ones saying things like, “you are lazy”, “you just want attention” or “you are a manipulator” , it will hurt the depressed person at their core. Many persons suffering from a depressive episode, are Not Lazy, more likely they are drained. Depression can cause insomnia and the person can go days without getting any more than a few hours of sleep. A person having a depressed episode is not being manipulative and yes they may be seeking attention. They are crying out for help.
KNOWING THE SIGNS AND SYMPTOMS
Beloved, depression is a serious issue within our communities. There are too many people who are suffering in silence or crying out for help that is going unnoticed. I am reminded of the late great actor Robin Williams who from an outward view had everything going for him. He had money, a great network of family and friends, an established career, yet he was living a personal hell and didn’t seek help, much to his demise. We need to know the warning signs and symptoms of depression for the mental health of ourselves and those we love. According to the National Institute of Mental Health symptoms of depression may include the following:
• Difficulty concentrating, remembering details, and making decisions
• Fatigue and decreased energy
• Feelings of guilt, worthlessness and/or helplessness
• Insomnia, early morning wakefulness, or excessive sleeping
• Irritability, restlessness
• Loss of interest in activities or hobbies once pleasurable
• Loss of interest in sexual intercourse (to include sexual dysfunction)
• Overeating or appetite loss
• Persistent aches or pains, headaches, cramps, or digestive problems that do not ease even with treatment
• Persistent sad, anxious, or empty feelings
• Thoughts of suicide or suicide attempts
BECOMING ONE WITH YOUR DEPRESSION CAN TURN YOUR LIFE UPSIDE DOWN
In hindsight, I realize that I was suffering from depression long before I was clinically diagnosed. I was able to do my every day functions and excelled at work receiving promotions and bonuses; however, I did not pay attention to my irritability, loss of energy, inability to sleep, and loss of sex drive. I meandered through life oblivious to what was going on inside my body and mind because the way I was living became my new normal. In other words, I adapted to my depression and depression became my norm. Getting help for my depression is one of the best things that I could have ever done for myself. I still have good days and not so good days, however, today I have far more good days than bad days. I first had to acknowledge that my life was spinning out of control and accept that I suffer with depression.
I made a conscious decision to seek help and I had to be willing to do whatever it takes to maintain my mental health. I have learned to put the oxygen mask on myself first, I was suffocating and dying with depression, while trying to help and fix everyone around me. Becoming more in tune with my feelings and emotions, allows me to notice when I am about to get into what I call a funk. I refocus, meaning, giving myself positive self-talk such as Salim don’t go there or purposely getting out of the house and engage in an activity or the company of family and friends who are uplifting. I am also mindful to schedule an appointment with my therapist immediately. I am comfortable with’ – ‘admitting’…. I may be in counseling for the rest of my life, if only for periodic check-ins or as I call them tune-ups.
Since I decided to seek counseling I can sing like Dr. Marvin Sapp “I am stronger, I’m wiser, I feel better, so much better”. I never could have made it, without a strong faith in Christ and the help from a therapist.
If you or a loved one is suffering with depression especially if it has been going on for a long period of time or experiencing any of the symptoms mentioned in the previous paragraph I suggest you make an appointment with your doctor or therapist to seek help or if you or your loved one has expressed suicidal thoughts or suicidal intentions do not hesitate to call the Suicide Hotline at (1-800-784-2433) or for TTY (1-800-799-4889).
Dr. Bilal-Edwards is an expert in youth development and social issues in an urban environment for men and boys of color. He has spoken in churches, at conferences, and retreats across the country as well as have conducted parent trainings and trainings to educators, social workers, youth workers, community organizations, and law enforcement officials. Dr. Bilal-Edwards specializes in counseling persons with co-occurring disorders and he is a highly respected relationship and life coach.
Contact: dr.salimbilaledwards@gmail.com
Confused about health care reform? You’re not alone. Click on the links below to get the facts about health insurance reform.
Affordable Care Act: Obamacare & Health Reform Facts: http://healthreform.kaiserpermanente.org/
Understanding the Impact of Obamacare on Medicare: http://blog.ehealthmedicare.com/media-center/infographics/?pid=11
What does Marketplace health insurance cover?
https://www.healthcare.gov/what-does-marketplace-health-insurance-cover/
Affordable Care Act: State-by-State Impact: http://www.hhs.gov/healthcare/facts/bystate/statebystate.html
The Lifestyle Revolutionaries Guide to Addiction Intervention: http://www.lakeviewhealth.com/InterventionGuide.pdf
Other Resources
http://www.whitehouse.gov/realitycheck/
http://factcheck.org/
Are We More Accepting Of Obesity In The Black Community?
By Gary A. Johnson
Americans are getting fatter and fatter by the year. There’s no other way to put it. Health and weight statistics for black Americans is even worse.
According to the publication Health, United States, 2013, 38% of black men in America are considered to be obese compared to 50.8 percent of African-American women. According to the U.S. Department of Health and Human Services, overweight or obese is defined as a Body Mass Index (BMI) of 25 pounds or more.
A 2013 study from the American Psychological Association reported that about 60 percent of black women are obese compared to 32 percent white women and 41 percent Latino women.
Carrying around those extra pounds increases the likelihood of developing Type II Diabetes and High Blood Pressure – two diseases that disproportionately affect the black community.
Being overweight also increases the risk of stroke, heart disease, arthritis and certain cancers. In fact, obesity could become more dangerous for your health than smoking cigarettes.
Yet, in the black community, many folks believe or have convinced themselves that being “big boned” is more acceptable. We need to STOP that thinking right now.
If you follow me on Facebook or Twitter, you have read about my struggle to lose weight. If you’ve ever visited my Instagram page, most of the pictures are of food that I cooked and then ate. I’m a damn good cook. I suffer for my food.
I am putting myself out there. I am obese and my condition developed as a result of making a serious of poor choices over the past 20 years. I went from weighing 195 lbs to my current weight of 310 lbs.
At one point I was carrying 324 lbs on this 6′ 4″ frame. Fortunately for me, my body has been good to me. I never smoked, used alcohol or drugs and I don’t drink sodas. My weakness is food. I am an emotional eater and I love to cook and eat.
Here I am “walking the trail” on top of the Woodrow Wilson Bridge at National Harbor on the DC side.
Lately, I’ve been able to reverse some of these negative health effects. Two years ago I gave up sugary fruit juice drinks. I drink mostly water, green smoothies or a combination of Braggs Organic Vinegar and water. If I drink tea, I don’t use sugar. I will start my day with low-sodium vegetable juice in place of Orange juice. These simple choices have made a difference in my health. My last blood pressure reading was 116/78. Not bad for a 300+ pound guy. I started exercising (cycling, walking and weights) consistently and stopped eating at fast food restaurants. I also started buying healthier and organic foods. This costs more but I think it’s worth it.
Make no mistake. I have a long way to go and need support. I have lost over 30 lbs 4 times over the last 15 years. The difference this time is that I am doing it sensibly (slow and steady). No fad or crash diets. Is it easy? No! Is it worth the pain and effort? Yes!
“Many African-American women view being obese as part of their culture,” says Thaddeus Bell, M.D., a family practitioner in South Carolina, in an online interview for icyou.com. It is understood within the African-American community that curvy, overweight women are considered more appealing to black men than normal- or under-weight women. There is almost a reverse distortion of body image – with thicker women fighting weight-loss and slender women wanting to gain weight in order to be accepted.
This may account for the staggering statistic that 4 out of 5 African-American women are overweight or obese. It is even more alarming that some of these women are making a choice to live at an unhealthy weight. African-American women of all ages report less exercise than their white counterparts. “Many of them feel that it’s not feminine or they’re afraid to sweat because it will ruin their hairstyle,” adds Dr. Bell.
Other hindrances include not having child care, not having enough time to be physically active, and not feeling safe being active in their neighborhoods.
African-American men aren’t off the hook either. African-American men also exercise less than white women, and have the highest prevalence of obesity among all male ethnic groups.
However, African-American men are more active than their female counterparts, which may be the reason that only 28.8 percent are obese, compared to 50.8 percent of African-American women.
There is an interesting video called “Dealing with Obesity in the Black Community” on YouTube by Walter Lee Hampton II. This is a no non-sense video about exercise, eating and living a healthier life. I would also recommend reading “Obesity and the Black American: Causes, Culture, Consequences, and Costs.”
Don’t Lose The War Of The Mouth
Dr. Fredrick D. Clark is not your average dentist. Dr. Clark is an “Oral Physician” and dental child care advocate who is on a mission. According to Dr. Clark, dental care cannot be relegated to the “out of sight, out of mind” category if one wishes to retain their teeth.
One of the primary reasons many of us do not get dental care is a lack of perceived need. Unfortunately the need may be present in spite of the absence of pain or apparent symptoms. Don’t loose the daily battles out of fear or apprehension, neglect or thinking that you know everything about your own teeth; you don’t. Only your dentist knows for sure. Don’t loose the war of the mouth.
Dr. Clark sat down with me for an impromptu exclusive video interview about preventive dental care. Please watch the video below and forward it to all of your friends and family.
For more information on Dr. Clark click here to visit his YouTube channel. Dr. Clark testified before Congress in 2007: http://reform.democrats.house.gov/documents/20070516164114.pdf. His first article on our blog is called “The War of the Mouth.”
By Fredrick D. Clark, D.D.S.
The battle is engaged. The combatants are tiny, but the war will be waged for decades. Unfortunately, it is a war, which will have many casualties. This is the war of the mouth. The enemy is PLAQUE, a colony or groups of numerous bacteria that live in the oral cavity. They are the culprits behind the many problems we experience with our mouths over the years. The battle begins with the eruption of the first tooth.
Plaque begins to attack the teeth and gums in our infancy and continues throughout childhood, teen years, adulthood and old age. We cannot see the enemy (plaque) until an appreciable amount builds up on the teeth and even then, it appears benign.
It does not hurt, in fact may even be unnoticeable, but it can lead to horrific consequences if left unchecked. Bad breath (halitosis), tooth decay (cavities), gingivitis (gum swelling, bleeding), periodontal disease (destruction of gum and bone) which causes tooth loss; all of these conditions are caused by the presence of plaque.
The teeth are just one part of a larger system, which includes the teeth and its supporting structures, the gums, the jawbones and the periodontal ligaments, (which hold the teeth to the bone). Collectively; this system is called the PERIODONTIUM.
Thus, all of the above mentioned conditions are diseases of the periodontium. The war I speak of is relentless and many of us lose the daily battles because it goes on painlessly. By the time one complains of a toothache, the damage is sometimes too extensive to save the tooth. Most people are familiar with cavities because they start at an early age in most children. There are a few things we can do to prevent cavities such as adequate brushing, daily flossing and most importantly, professional dental cleanings and checkups. This is a two-fold approach of (1), home care and (2), help from your Dental Professional in early detection and treatment.
I like to relate cavities to a concept most can understand; a cavity is like a cancer growing in which if left untreated will get larger and eventually destroy the tooth. Not only can it get larger but can cause immense pain, jaw swelling, abscesses, pus formation; and, the longer you wait the worse it gets. The results of many years of neglect is what causes people to require expensive dental care such as root canals, caps or crowns, extractions and dentures. Before it is too late, schedule an appointment with your dental professional; an ounce of prevention is worth a pound of cure. Learn how to win the battle of the mouth. You can keep your teeth for a lifetime; the key to keeping your teeth is early detection and treatment long before the problem becomes painful.
Dental care cannot be relegated to the out of sight, out of mind category if one wishes to retain their teeth. One of the primary reasons many of us do not get dental care is a lack of perceived need. Unfortunately the need may be present in spite of the absence of pain or apparent symptoms. Don’t lose the daily battles out of fear or apprehension, neglect or thinking that you know everything about your own teeth; you don’t. Only your Dentist knows for sure. Don’t lose the war of the mouth.
5 Things Young African-American Women Can Do To Cope with Breast Cancer
Learning that you have breast cancer can be one of the most shocking and life altering moments of your entire life. The initial diagnosis can bring on feelings of not only worry, but life’s fragility. The idea of time being precious no longer seems like something that you just say in passing when talking to friends. Your time really does become precious and your sense of purpose kicks into over drive. Breast cancer is affecting more young African-American women each year and the ages continue to get younger and younger. But the diagnosis, the treatment, and the recovery do not have to be a grim experience. Yes, it’s extremely hard and will probably be the hardest thing you will ever have to go through in your life. Questions may arise such as: how did this happen to me? Why me? And what am I going to do now? I had all of these same questions after all, I was only 31 years old, African-American, and in good health. These are all common concerns among women who have been diagnosed with this disease, but more important than the initial shock and the treatment and even surgery is the mental state of the woman after she learns that she has the disease. For every woman who has just learned that she has breast cancer and for every woman who knows another who has been diagnosed there are five rules that we must all follow in order to ensure that our lives and the lives of our loved ones will be fulfilled while we take this journey.
1) Focus on getting better. Spend very little time thinking about the disease itself, rather, spend time thinking about your life after you get better. I had a nurse to admit to me that people get sicker when they spend too much time in the hospital worrying about their illness.
2) Avoid morbid, pessimistic people. Even people who you love and who love you can become a drain on your spirit when they spend too much time treating you like your diagnosis is an automatic death sentence. Many people recover from cancer and go on to lead happy, healthy, and fulfilling lives.
3) Change your diet. Don’t accept any of the soda, sweets, and other junk foods offered to you at your cancer treatment center or anywhere else. A low/no dairy, low/no sugar, no alcohol, and junk free diet helps your body to fight against the tumor while you are going through conventional treatments. Drink plenty of water, eat extra servings of fresh vegetables, and add extra fiber to your diet to cleanse your body.
4) Keep doing what you. The initial diagnosis will be a serious blow and the chemotherapy treatments and surgery will knock you off your feet for a while, but keep your eyes on the prize. Staying focused on your family life (esp. your children) helps you to maintain a positive and healthy mental state. A positive and healthy mental state also helps your body to fight against the cancer and to recuperate from the toxicity of chemotherapy. The entire time that I have been going through treatments, I have been a single mother, a sociology student, a freelance writer and author, and a small business owner. I never missed a beat (except the days when I was ill from the chemo) because I chose to continue living and thriving.
5) Pray, meditate, chant, or whatever it is that you do. Your mind needs to be cleansed when going through a battle with breast cancer. Your spirit should always be nurtured so that you may receive divine guidance. Spend little time sobbing in prayer and more time focused on what you want your outcome to be. Love yourself, visualize your body healing, and trust that things will work out as they should.
As a breast cancer patient and self-proclaimed ‘survivor’ of the disease, I know all too well what a woman goes through after she gets that call from the doctor’s office. Some women choose to immediately join support groups and notify their family members. There are other women who decide that the best way to deal with the disease and the forthcoming recovery, is to cope in solitude and in silence. I was one of those women. As a breast cancer patient enduring the most toxic of chemotherapy treatments in conjunction with a few naturopathic treatments, I have learned that my immediate state of mind and well-being contribute greatly to the way that my body has responded to the treatments and how well I am doing physically while on the road to recovery. Throughout this transition I came up with five ways to cope with the disease so that may have the best outcome while on the road to recovery.
About The Author
Zekita Tucker is freelance writer and the author of ‘Your Story Book One.’ Her articles have been published by many national and international publications and she has been featured by ABC World News and the Roland S. Martin radio show. To learn more please visit www.zeniampublications.com.
Here are some helpful links to learn more about breast cancer and breast cancer prevention.
National Breast Cancer Foundation
Black Women’s Health Imperative
African American Breast Cancer Alliance
Cancer Facts and Figures for African Americans
We recommend that you check out the website Healthyblackmen.org which is an online health and lifestyle resource for black men. Their mission is to increase health awareness and overall health literacy to help inform health decisions for black men everywhere.
12 Things Your Dentist Wants You to Know
























 Kristen Baker-Geczy is a communications specialist, active duty military spouse, and former MWR marketing coordinator. She was also deployed to Southwest Asia as an Air Force contractor.
Kristen Baker-Geczy is a communications specialist, active duty military spouse, and former MWR marketing coordinator. She was also deployed to Southwest Asia as an Air Force contractor.
































































I am Tiffiney Neal and I have lost over 275 pounds, basically two human beings from my body. I have the proof of the photos with the dramatic change of lifestyle that I had to partake in. It was during a ten year span of battling diabetes, not being able to play with my kids and having trouble finding my size of clothes in retail stores. Right now, it feels SOOOO good to walk into a fashion store and have the ability to pick any clothes that are sexy, luxurious and comfortable in my skin. In the past, I used to cry when I leave the store because I would see something that I liked but could not wear it because I was too heavy or the salesperson would tell me that they don’t have my size.
It used to hurt me to the CORE and people do not understand how much pain that I feel when this happens. So, I decided ENOUGH is ENOUGH! I want to be healthy! I want to live longer than the doctors tell me! I want to defy the odds and achieve the weight loss! I want to be HAPPY!
The bottom line is that I lost over 275 pounds! And still losing! I was once tipped the scales at over 400 pounds, but now I am a healthy and happier 160 pounds with a 5 foot 6 inch frame! My motivation is when people used to talk about me because of my weight and I just got sick and tired of it! I will not tolerate any more abuse and I am going to do something about it. I exercised 5-6 days a week, for 2 hours. I substituted on odd days to perform cardiovascular fitness such as the treadmill and elliptical, and my even days, I did some strength and abdominal training. On my days on which I couldn’t run, I did a brisk walk for 3 miles. When I did run, I ran my heart out! I was my own inspiration! I needed to lose the weight badly and pursue my goal, so when I put my mind into something, you better believe I will follow through on it. I wanted to give up so bad and just let God take me, the problem that God wasn’t ready for me just yet. He told me that I still had a lot of work to do and I will help you through it.
It was a complete lifestyle change, I have started to eat more healthier such as fruits and vegetables, ate more protein and less carbohydrates. Stayed physically active by working 6 days a week and going to the gym on my free time. Also, I liked to dance as well, dancing believe it or not is a great tool for burning calories and having energy.
My advice for those that want to lose the weight is to start off slow. The body will not lie to you, it only can do what is capable at that moment. So don’t force yourself, don’t push yourself to do so much more that you would end up hurting yourself and fall further behind your goal. The key is about setting goals is to give yourself a timeline on how much to lose in a week, a month, 6 months, etc. Be accountable for yourself, don’t make any excuses and be prepared for setbacks…..you will have them. The resilient ones are the ones that can overcome the bad days and turn them into positive, fulfilling great days!
Right now, I am a model, known as Amor Mz Hollywood. My website is amormzhollywood.com and I looking to share my story to the world and to make a difference in somebody’s life. I feel great, inspired, motivated and fabulous! It was a long road but I believe I am much closer to my journey than ever before in my life!
XOXO
Amor Mz Hollywood
(Tiffiney Neal)
[…] Click here to visit our Health and Wellness page to stay healthy, wealthy and wise. […]
[…] HEALTH & WELLNESS […]